Because asparaginase is used exclusively in ALL, most adult oncologists do not administer it routinely.

Because asparaginase is used exclusively in ALL, most adult oncologists do not administer it routinely.

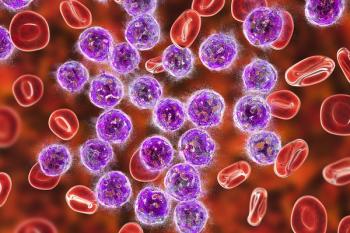
Nearly 20% of patients with multiple myeloma have a form of the disease in which they make high quantities of a component of monoclonal proteins, which damages the kidneys.
Investigators find a precision medicine that can identify those with the rare disorder who may benefit from FDA-approved siltuximab.

The FDA has approved a second drug, zanubritinib, for the treatment of adult patients with Waldenström’s macroglobulinemia.

Lab values for sodium, potassium, chloride, magnesium, BUN, creatinine, glucose, and CO2.
Approved indications for idelalisib include relapsed chronic lymphocytic leukemia, small lymphocytic lymphoma, and follicular B-cell non-Hodgkin lymphoma.
The mutated genes in question, TET2 and DNMT3A, each influence the efficacy of treatment in different ways.

This designation could shorten the FDA review period to 8 months compared to the 12 months under Standard Review.
Alexandra S. Wolff, PharmD, BCOP, comments on her experience with CPX-351 in clinical practice and the potential to combine CPX-351 with targeted agents for AML.
Alexandra S. Wolff, PharmD, BCOP, explores the 5-year follow-up data from the phase 3 trial of CPX-351 in AML.
Expert continues discussion on important considerations for the optimal use if venetoclax in patients with AML, such as CYP3A4 and p-glycoprotein drug interactions.
Alexandra S. Wolff, PharmD, BCOP, highlights considerations for optimal use of venetoclax in patients with AML, such as tumor lysis syndrome prophylaxis.
Expert discusses the role of venetoclax in the treatment of AML and if achievement of MRD negativity can be used to predict long-term outcomes.
Expert continues discussion of IDH1 and IDH2 inhibitors in AML and examines prioritization of IDH1 and IDH2 inhibitors versus venetoclax in newly diagnosed AML.
Tisagenlecleucel is a CD19-directed genetically modified autologous T cell immunotherapy already indicated for B-cell precursor acute lymphoblastic leukemia and diffuse large B-cell lymphoma.
Alexandra S. Wolff, PharmD, BCOP, discusses use of IDH1 and IDH2 inhibitors in newly diagnosed AML patients and highlights recently released trial data.
Expert examines the status of second-generation FLT3 inhibitors in newly diagnosed AML patients and the challenge with comparing clinical trial efficacy endpoints.
Expert discusses the role of FLT3 inhibitors in the treatment of AML and if benefit from midostaurin in combination with chemotherapy can be predicted.
Between 40% and 50% of patients respond long term without relapsing.

Rivaroxaban is the first and only therapy indicated for both coronary artery disease and peripheral artery disease.
Rylaze was granted Fast Track Designation by the FDA in October 2019 for acute lymphoblastic leukemia and was approved as part of the Real-Time Oncology Review program.
When direct oral anticoagulants are taken, especially for the first time, patients may be at risk of bleeding.

The FDA has granted orphan drug designation to CFT7455 for the treatment of multiple myeloma, according to a press release from manufacturer C4 Therapeutics.

Physicians may ask for either or both of comprehensive metabolic panel or complete blood count tests every 3 to 6 months, based on the conditions patients have.
Daratumumab and hyaluronidase-fihj (Darzalex Faspro, Janssen) was approved in July in combination with pomalidomide and dexamethasone for the treatment of patients with multiple myeloma following their first or subsequent relapse.