Lymphoma
Latest News
Latest Videos
CME Content
More News
Denileukin diftitox-cxdl is the only therapy approved for cutaneous T-cell lymphoma that targets IL-2 receptors in malignant T-cells and Tregs.
Replacing carmustine with cisplatin in BEAM ((carmustine, etoposide, cytarabine, and melphalan) conditioning could be more cost-effective for patients.
Investigators determine the efficacy and safety of the combination in a 2-phase trial.
The new approach could optimize precision medicine and lead to better outcomes across a variety of disease states.
In a study of Swedish patients with mantle cell lymphoma, the participants faced a heightened risk of infection after their diagnosis and associated treatment for the disease.

Individuals with tattoos were found to have a greater risk of developing malignant lymphoma, with the risk being highest within 2 years of receiving a tattoo.
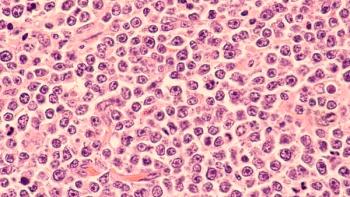
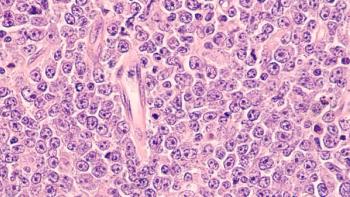
Mutations in KLHL6 Associated With Tangible Disease Characteristics in Diffuse Large B-Cell Lymphoma
Researchers found that certain mutations in KLHL6 can lead to an increase in the number of B-cell receptors, resulting in poor outcomes for patients with diffuse large B-cell lymphoma.

The results are promising for patients with relapsed or refractory follicular lymphoma and diffuse large B-cell lymphoma, and the trial is ongoing to assess the efficacy of odronextamab in other subtypes.

Increased immunoglobulin replacement therapy led to reduced infections and managed secondary immune deficiencies such as hypogammaglobulinemia.
Combining multiple drugs to induce a deep response in patients with diffuse large B-cell lymphoma could open curative pathways for those affected.
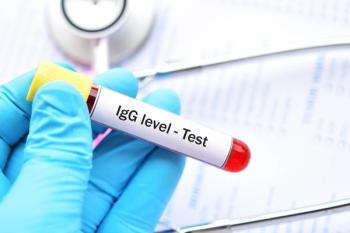
An increased frequency of immunoglobulin G testing in patients with chronic lymphocytic leukemia (CLL) and non-Hodgkin lymphoma (NHL) was also associated with a lower likelihood of severe infections.
The approval marks the first and only T-cell engaging bispecific antibody administered subcutaneously to treat patients after 2 or more lines of systemic therapy.

There are numerous challenges with cell and gene therapies in oncology, such as accessibility, cost, and prior authorizations, as well as the need for improved education and training within the oncology community.
Tim Mok, PharmD, BCOP, BCPS, discusses innovative therapies that are changing the treatment options available for patients with hematologic malignancies.

Compared with standard of care chemoimmunotherapy, acalabrutinib with bendamustine and rituximab reduced risk of death or disease by approximately 27%.
Participants in the study had durable response for over 1 year, in addition to positive efficacy indicators.
Zanubrutinib shows potential in treating patients with treatment-naïve high-risk chronic lymphocytic leukemia and/or small lymphocytic lymphoma with del(17p) and/or TP53 mutation.
Brentuximab vedotin in combination with lenalidomide and rituximab had a favorable safety profile for patients with relapsed/refractory diffuse large B-cell lymphoma.
Lisocabtagene maraleucel is being investigated for mantle cell lymphoma, relapsed or refractory (R/R) large B-cell lymphoma, and R/R follicular lymphoma.
Lisocabtagene maraleucel (Breyanzi; Bristol Myers Squibb) is a CD19-directed CAR T-cell therapy that is delivered as a one-time infusion.

Previously, glofitamab had received an accelerated approval for patients with relapsed or refractory diffuse large B-cell lymphoma who received 2 or more prior lines of systemic therapy.
The antibody drug conjugate was used in combination with the anti-cancer drug SG3249, and demonstrated efficacy in mouse models after 1 week.

There are unique complexities when implementing bispecific antibodies, including site of care considerations, monitoring, and management of adverse events.
These FDA-approved therapies are used to treat lymphoma after 2 or more lines of therapy and represent significant advancements in the treatment of lymphoma.
The mutation impacts BAF proteins and can lead to progression of follicular lymphoma, according to the investigators.