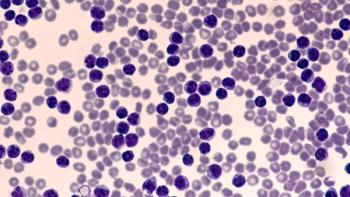
Chronic Lymphocytic Leukemia: Considerations for Anti-CD20 Monoclonal Antibodies
Anthony Perissinotti, PharmD, BCOP, explains potential scenarios requiring anti-CD20 monoclonal antibodies as a therapy for chronic lymphocytic leukemia.
Episodes in this series

Kirollos Hanna, PharmD, BCPS, BCOP: Mr Perissinotti, in your practice, what would it be a good clinical scenario to incorporate an anti-CD20 monoclonal antibody?
Anthony Perissinotti, PharmD, BCOP: I agree with everything you said. For any patient who’s receiving venetoclax, I would. If you’re following the CLL14 study, and you’re trying to get deep remissions, and you want to keep your patient off therapy for as long as possible, the anti-CD20 and obinutuzumab are going to deepen your remission. Venetoclax is an absolute. Even MURANO used rituximab. It’s a little less clear whether you need rituximab or obinutuzumab in the relapse setting, especially if you already previously received it. Let’s follow the data.
With the BTK inhibitors, there isn’t any clear guidance from the literature as to who’s going to benefit from a monoclonal antibody. Open questions are, did the Alliance [for Clinical Trials in Oncology] trial have no difference because rituximab [Rituxan] was the problem? Did you need to use obinutuzumab, something with more antibody-dependent cellular cytotoxicity [ADCC]? Maybe it’s ibrutinib, which inhibits ITK and can reduce ADCC and inhibit the mechanism of rituximab. Maybe you shouldn’t use a monoclonal with rituximab. Being able to compare, contrast, and extrapolate whatever happened with rituximab or ibrutinib with obinutuzumab and acalabrutinib is tough.
The ELEVATE-TN trial pretty much tells you the story: there’s a very marginal benefit. Even at the 4-year update that was recently published, it’s a marginal benefit. I agree completely with you with COVID-19: going in and out of the hospital is not ideal. Vaccine responses with obinutuzumab are next to nil. That’s not ideal for our patients.
Going back to your question of where I would consider using it: with a BTK inhibitor. If I have a patient with CLL [chronic lymphocytic leukemia] with a tremendously high white blood cell count—let’s say they present with a white blood cell count of 700,000 per mm3—that patient is going to have lymphocytosis from their acalabrutinib or ibrutinib, and it’s going to skyrocket to into the millions. That makes me a little concerned. I want to debulk that patient to bring it down as much as possible. It freaks me out. Clinically is that going to end up leading to leukostasis or tumor lysis? Probably not. But it would make me feel a lot better if the white blood cell count wasn’t rising to the millions. That’s 1.
If I have a patient who needs a quick response—they have really painful lymphadenopathy, or they’ve got a packed marrow and pancytopenia—and I think a BTK inhibitor is appropriate, and I might consider using obinutuzumab in that setting as well. It’s not evidence based at all; it’s anecdotal of what I do. That’s that teeny-tiny percent—99% of my patients would not get an anti-CD20.
Transcript edited for clarity.
Newsletter
Stay informed on drug updates, treatment guidelines, and pharmacy practice trends—subscribe to Pharmacy Times for weekly clinical insights.