Intravenous immunoglobulin prescriptions deemed non-compliant according to French national guidelines were more common in younger patients.
Intravenous immunoglobulin prescriptions deemed non-compliant according to French national guidelines were more common in younger patients.

Results demonstrating safety and efficacy in those with anemia in non-dialysis dependent chronic kidney disease and anemia in dialysis-dependent chronic kidney disease were presented at the 2024 American Society of Nephrology Kidney Week.

This approval marks the first and only anti-tissue factor pathway inhibitor approved in the US for the treatment hemophilia A or B, and the first approved hemophilia treatment to be administered via a pre-filled, auto-injector pen.
By utilizing a lower dose, patients can avoid potential adverse events and high financial burden.

Eculizumab (Soliris; Alexion), a C5 inhibitor preventing cleavage into C5a and C5b, is widely considered the first-line therapy for high-risk TA-TMA.

Luspatercept reduced the need for transfusion in patients with myelofibrosis (MF).
Two groundbreaking cell-based gene therapies, exagamglogene autotemcel and lovotibeglogene autotemcel, were recently approved by the FDA for the treatment of sickle cell disease.
Treatment advancements highlight the curative potential of bone marrow transplants and emerging gene therapies.

Inflammatory conditions such as celiac disease can require care consideration and monitoring to manage iron deficiency

The investigational drug achieved non-inferiority compared to routine Factor VIII.

These findings build off research from March 2023 that demonstrated efficacy and safety of renizgamglogene autogedtemcel in patients with sickle cell disease.
Mim8 had a safe and well-tolerated profile, with no deaths or thrombotic events reported for patients with hemophilia A.

A 1-time infusion of valoctocogene roxaparvovec had demonstrated sustained bleed control and factor VIII expression in patients with hemophilia A.
Patients with sickle cell disease with more than a 6-month delay transitioning from pediatric to adult care were about twice as likely to be hospitalized.
Antihemophilic factor (recombinant) Fc-VWF-XTEN fusion protein-ehtl was initally approved in February 2023 for adults and children with hemophilia A for prophylaxis and on-demand treatment to control bleeding.

With gene therapy, anti-tissue factor pathway inhibitors, and RNA interference therapy targeting antithrombin, there are many new options that will be available for the patients impacted by hemophilia.

The 1-time treatment may be a better alternative for patients who don’t want to undergo frequent doses of standard of care intravenous factor IX infusions.

The orphan drug designation (ODD) comes after positive results from a phase 2 trial that showed cevidoplenib improved platelet counts by 63.6% and 40.9% in 2 different dose groups.
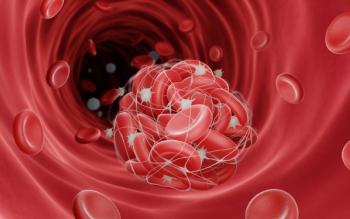
These disorders can be fatal, making pharmacists’ role in detection crucial.

Most patients with myelofibrosis will develop anemia over the course of the disease, with more than 30% discontinuing treatment as a result.
Corticosteroids are first-line therapy for gaining platelet stability but should only be used short term.

The findings, published the New England Journal of Medicine, showed treatment with rilzabrutinib led to a rapid, durable increase in platelet count while supporting an acceptable safety profile.

Study results showed that an individual with the blood disorder did not respond to treatment, including intravenous immunoglobulin, following their second dose of the Pfizer vaccination.
Experts say the COVID-19 pandemic may create a shortage of plasma therapy.

This activity is supported by educational grants from Dova Pharmaceuticals, INC. and Cure Media Group.