The Effects of COVID-19 on DED
The panel reflects on the effects COVID-19 has had on their patients with dry eye disease.
Episodes in this series

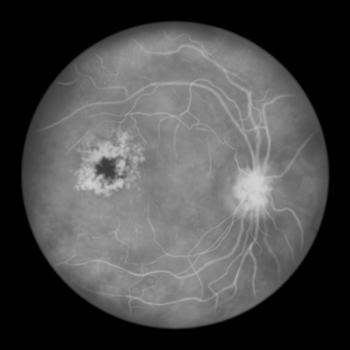
Lisa M. Nijm, MD, JD: Unfortunately, I have seen more patients suffering from dry eye disease since the COVID-19 pandemic [began], and it makes sense. We’ve all done exactly what we’re doing right now. Everybody is on computers all day, on phones, on iPads. We can’t get away from it. Kids’ screen time has increased dramatically with virtual school and everything else. I’ve certainly seen an uptick [in dry eye] during the pandemic, and I’ve seen it across all age groups. That’s the other thing. Often, we think of dry eye disease in older patients, but it’s actually across the board. It’s becoming more frequent among younger patients because we have other triggers that we’re looking at with effects of the pandemic—increased screen time and greater use of electronic devices along with all the normal things that go on (eg, allergies, wind, inflammatory diseases).
Brian Walker, RPh: Dr Nijm, I wanted to add to that. Since COVID-19 hit, there are a number of people who have increased medication use. Several medications cause dry eye. Since this pandemic, a lot of people have started antianxiety medications and sleeping medications, both of which can cause dry eye disease or cause a problem with dry eye. Also, a number of antidepressants have antihistaminic properties, and there’s been an increase in the number of people who have been taking antidepressants. We’re past spring, but during the summer, we still have a number of people who are allergic to grass and pollens coming out. We’ve had a wet spell over these past couple of weeks, so mold [levels] are also high. [In addition, many] people take antihistamines like Claritin; Claritin and Zyrtec are the 2 that cause [dry eye] the most, in addition to Benadryl. All of those drying products can increase the incidence of dry eyes.
Lisa M. Nijm, MD, JD: That’s such a great point, and thanks for adding to that because we sometimes miss or don’t pay close attention to [those crucial things]. You also reminded me of one of the other features of the pandemic that has increased dry eye disease, and that’s wearing masks. There is a phenomenon called MADE [Mask-Associated Dry Eye syndrome]. The way that masks sit on the face [may cause] some air to recirculate from the mouth and hit the eyes to cause more dryness.
I know of at least 1 paper that was published [involving the] greater incidence of chalazia and styes on the eyelids, and there [may be] an association between all of that and bacteria coming from the mouth and being recirculated to the eye. [The authors] advocated for [the use of] more mouthwash and more stringent mouth hygiene to help with lid hygiene and reduce incidence of chalazia and dry eye. Everything that you mentioned—increased [use of] medications, wearing of masks—are excellent reasons why] dry eye has worsened during the pandemic.
Brian Walker, RPh: When I work my 12-hour day and have my computer glasses on with the mask, by the time that I’m at hour 10, my eyes are very dry. It doesn’t seal as well or for as long as it should. [This is experienced by] medical professionals who have to wear those masks.
Transcript edited for clarity.
Newsletter
Stay informed on drug updates, treatment guidelines, and pharmacy practice trends—subscribe to Pharmacy Times for weekly clinical insights.