
Plozasiran shows promise in reducing cholesterol and triglyceride levels in patients with mixed hyperlipidemia and other harmful conditions, addressing significant cardiovascular risks.

Plozasiran shows promise in reducing cholesterol and triglyceride levels in patients with mixed hyperlipidemia and other harmful conditions, addressing significant cardiovascular risks.

The fixed-dose combination yielded a 49% greater reduction in low density lipoprotein cholesterol (LDL-C) compared with placebo.
Experts provide guidance on managing high cholesterol in adults older than 75 years, emphasizing personalized care and shared decision-making for optimal outcomes.

A significant number of patients with high low-density lipoprotein (LDL) cholesterol lack prescribed lipid-lowering medications, highlighting gaps in treatment and care practices.

Lepodisiran, a small interfering RNA, demonstrated cholesterol-lowering effects at 16-mg, 96-mg, and 400-mg doses, with the highest dose being the most effective.

When used in combination with background statin therapy, AZD0780 resulted in major reductions in low-density lipoprotein cholesterol (LDL-C) and achievements of guideline-recommended LDL-C goals.

Notably, high levels of high-density lipoprotein cholesterol (HDL-C) were not associated with the risk of dementia following adjustments for triglyceride levels.
These results align with those from shorter-term analyses of low-density lipoprotein cholesterol (LDL-C) reductions with evolocumab and cognitive impairment risk.

Low-density lipoprotein cholesterol value below 88 mg/dL was associated with heightened mortality, highlighting the need for more liberal cholesterol targets in this population.
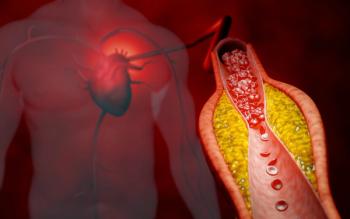
Non-high-density lipoprotein cholesterol was found to be more effective at predicting cardiovascular events such as stroke, myocardial outcomes, heart failure, and others compared with low-density lipoprotein cholesterol.

Alcohol consumption, though typically associated with adverse health outcomes, could be associated with reduced low-density lipoprotein cholesterol (LDL-C) and improved high-density lipoprotein cholesterol (HDL-C).
Sarcopenia, a progressive skeletal order that involves the accelerated loss of muscle mass and function, is associated with adverse outcomes such as functional decline, frailty, and mortality.
The results act as a contradiction to conventional wisdom of high-density lipoprotein (HDL) cholesterol being healthy and lowering the risk of heart disease, but more research is warranted.
Compared with other indicators of cardiovascular risk, the ratio of non-high-density lipoprotein cholesterol (HDL-C) to normal HDL-C had a stronger association with the risk of hypertension and heart disease.

This marks the first FDA-approved treatment for this rare lipid storage disease.

There was an association observed between fluctuating low-density lipoprotein cholesterol and the risk of developing dementia and cognitive impairment.
The agency will now review the novel PCSK9 inhibitor for possible approval in patients with or at high risk of atherosclerotic cardiovascular disease.
An inverse relationship was observed between genetic conditions associated with high levels of low-density lipoprotein cholesterol and the risk of developing T2D.
The results highlight hemoglobin A1c/high-density lipoprotein cholesterol as a potential clinical marker for long-term stroke risk.

High-density lipoprotein cholesterol, total cholesterol, and apolipoprotein B did not have significant correlations with chronic obstructive pulmonary disease.
Challenges include therapy gaps, nonadherence, and fragmented care.
This case report depicts a probable infusion reaction in a 61-year-old woman prescribed evinacumab for the treatment of familial hypercholesterolemia.

Regardless of confounding factors, the ratio of high-sensitivity C-reactive protein to high-density lipoprotein cholesterol predicts the all-cause long-term mortality.
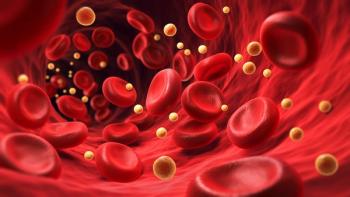
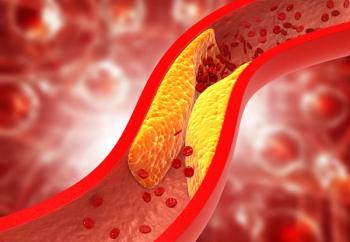
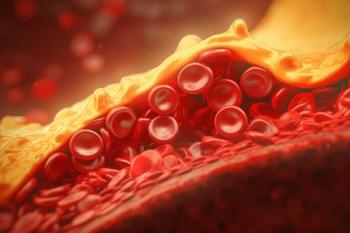
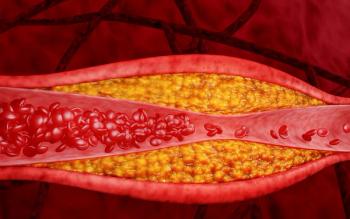
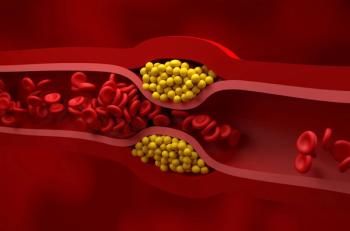
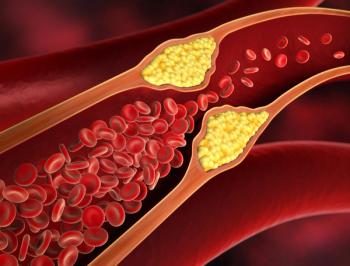
Dyslipidemia is a condition in which there are abnormal levels of lipids in the blood stream, including high levels of low-density lipoprotein cholesterol, low levels of high-density lipoprotein cholesterol, and/or high levels of triglycerides.
Patients with acute coronary syndrome who were in the high quartile were at significantly higher risk for major adverse cardiovascular events (MACE).