
For the first time, one antiplatelet agent has been recommended over another for non"ST-segment elevation acute coronary syndrome.

For the first time, one antiplatelet agent has been recommended over another for non"ST-segment elevation acute coronary syndrome.

Evolocumab cut low-density lipoprotein cholesterol levels by 60%, on average, in patients with heterozygous familial hypercholesterolemia

Live medication therapy management (MTM) reduces low-density-lipoprotein cholesterol significantly more than standard, chart-review MTM.

The results of an FDA safety review of omalizumab (Xolair) suggest the asthma drug slightly elevates the risk of serious cardiovascular and cerebrovascular adverse events.

In a Phase 3 study, odanacatib significantly reduced the risk of osteoporotic fractures, but it also might have contributed to major cardiovascular events.

Approximately 6.5 million Americans are prescribed digoxin, a cardiac glycoside with a long, fascinating history.


Wine consumption is cardioprotective, but only in patients who exercise, according to a new study.

Providing prescriptions when patients are discharged from the hospital after a stroke improves medication adherence, the results of a study suggest.

Aspirin may reduce the risk of blood clots in patients who cannot use traditional anticoagulants, new research suggests.
Several new anticoagulants have entered the US market in recent years, but research to find reversal agents for these drugs is ongoing.

Digoxin increases risk of death in patients with newly diagnosed atrial fibrillation.

Researchers evaluated more than 2 decades of evidence on atrial fibrillation patients taking vitamin K antagonists.

Researchers evaluated the risk of cardiovascular outcomes in atrial fibrillation patients with a history of falls.


A recent investigation found a significant increase in hospitalization rates for patients with atrial fibrillation in the United States.

When nonwhite heart attack patients were able to obtain cardiovascular medications without a copayment, their readmission rates for a major vascular event or coronary revascularization dropped significantly.

Current and recent users of nonsteroidal anti-inflammatory drugs were significantly more likely to develop atrial fibrillation, according to the results of a new study.

Trial finds that spironolactone significantly reduced hospitalization for heart failure in heart failure patients with a preserved ejection fraction but failed to decrease the incidence of the trial's primary composite outcome.

The results of a new study suggest that statin patients may have a false sense of security, leading them to believe the medication can offset the effects of a poor diet and lack of exercise.

According to a recent study, one-fifth of those aged 60 or older who were candidates for pharmacologic therapy under JNC 7 would rely on lifestyle blood pressure control under JNC 8.

The Target: Stroke initiative reduced the time before acute ischemic stroke patients were treated with intravenous tissue plasminogen activator, leading to reduced rates of in-hospital mortality and intracranial hemorrhage.

New atrial fibrillation treatment guidelines from the American Heart Association and American College of Cardiology clarify the role of novel oral anticoagulants and rate/rhythm control medications.
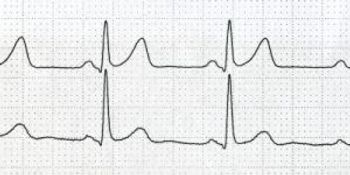
New guidelines from the American Heart Association, American College of Cardiology, and Heart Rhythm Society address use of new oral anticoagulants as well as warfarin to treat atrial fibrillation.

Patients who self-monitored their international normalized ratio weekly achieved significantly better control than those who did so less frequently, but all home monitoring patients performed well, according to a new study.