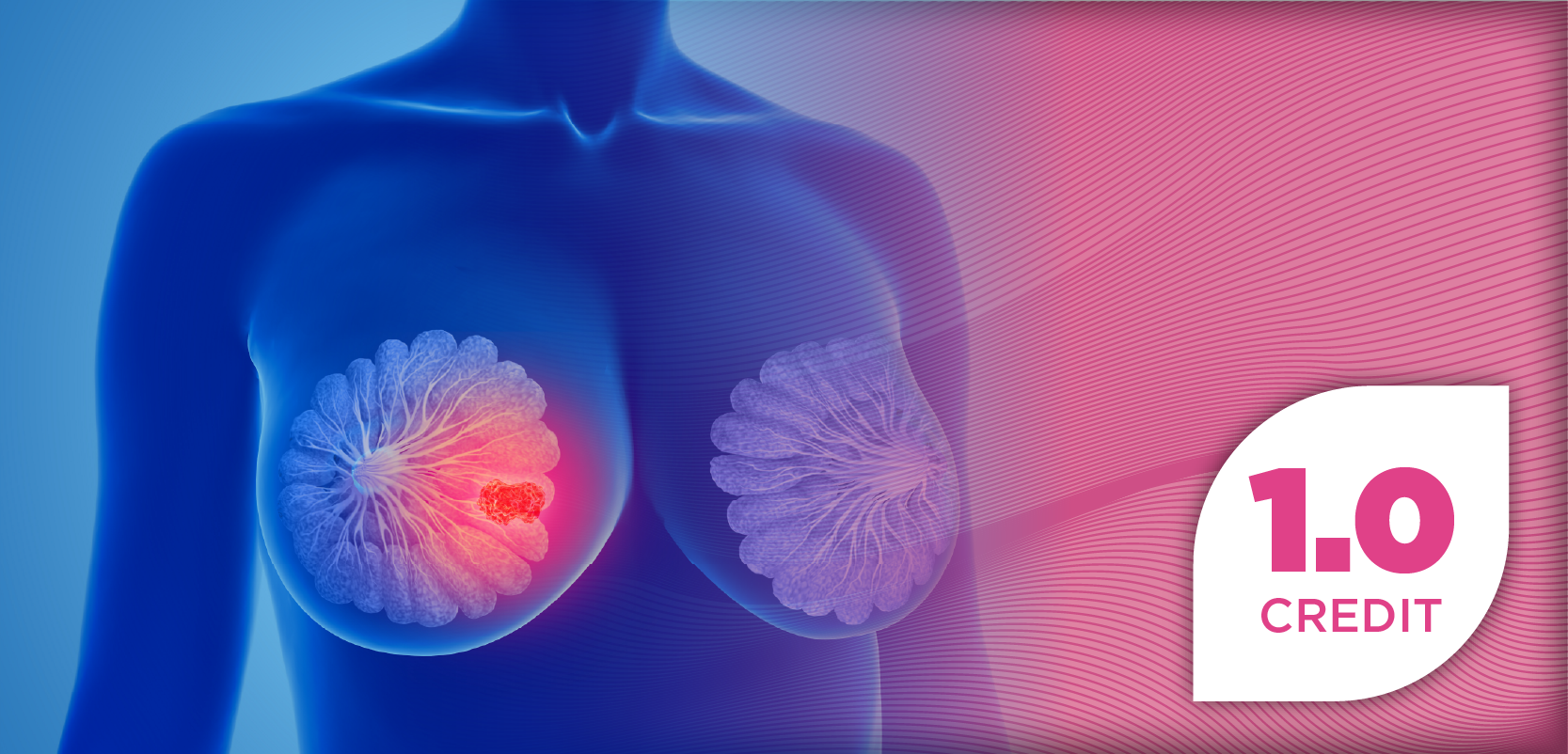
Pembrolizumab Before/After Surgery Improves pCR, EFS for Early TNBC
The addition of the immunotherapy pembrolizumab (Keytruda) to standard presurgical chemotherapy improved pathological complete response (pCR) rates for patients with triple-negative breast cancer (TNBC).
The addition of the immunotherapy pembrolizumab (Keytruda) to standard presurgical chemotherapy improved pathological complete response (pCR) rates for patients with triple-negative breast cancer (TNBC). Moreover, the continuation of pembrolizumab following surgery also showed early signs of improvement in event-free survival compared with placebo, according to findings from the KEYNOTE-522 study presented at the ESMO Congress 2019.
“The data suggest that the improved pathological complete response with pembrolizumab translates into fewer recurrences,” lead study author Peter Schmid, MD, PhD, from the Barts Cancer Institute, Queen Mary University, said in a statement.
The KEYNOTE-522 trial randomized patients with TNBC in a 2:1 ratio to receive pembrolizumab at 200 mg every 3 weeks (n = 784) or placebo (n = 390). All patients received 4 cycles of carboplatin plus paclitaxel followed by 4 cycles of doxorubicin or epirubicin plus cyclophosphamide. Following surgery, adjuvant pembrolizumab was continued for 9 cycles or until disease recurrence or unacceptable toxicity. EFS and pCR were dual primary endpoints for the study.
"Triple-negative breast cancer is a very difficult disease. Until now, we've struggled to have targeted therapies. Most of the treatments include chemotherapy," said Schmid. "It is well established that if you give chemotherapy before surgery for early triple-negative breast cancer that those patients where the cancer disappears, what we call a pathological complete response, those patients have a long-term benefit."
The pCR rate was 64.8% with pembrolizumab plus standard neoadjuvant chemotherapy compared with 51.2% for chemotherapy alone, showing a statistically significant improvement with the PD-1 inhibitor (P = .00055). In the PD-L1—positive group (CPS ≥1), the pCR rate was 68.9% compared with 54.9%, for pembrolizumab and placebo, respectively. This was equivalent to a 14.2 percentage point increase (CI, 5.3-23.1). In PD-L1–negative patients, the pCR rate was 45.3% with pembrolizumab versus 30.3% for placebo, a 18.3 percentage point increase (CI, -3.3 to 36.8).
After a median of 15.2 months of follow-up, an early benefit in event-free survival (EFS) had also emerged. For the early EFS analysis, 7.4% of events had occurred in the pembrolizumab arm compared with 11.8% in the placebo group. In the pembrolizumab group, the EFS rate was 91.3% compared with 85.3% with placebo; however, this benefit was not yet statistically significant (HR, 0.63; 95% CI, 0.43-0.93).
"There's already a difference between the two curves. We will have subsequent event-free survival analyses coming out soon,” said Schmid.
At least 1 treatment-related adverse event (AE) of any grade was experienced by patients in both arms during the presurgical phase. Grade 3 to 5 treatment-related AEs occurred at similar frequencies in the 2 groups, with 76.8% in the pembrolizumab arm compared with 72.2% in the placebo group. AEs led to discontinuation of any drug for 24.5% of patients in the pembrolizumab group compared with 13.1% for the placebo arm.
The most common treatment-related AEs for pembrolizumab and placebo, respectively, during the presurgical phase were nausea (62.7% vs 63.2%), alopecia (60.3% vs 56.6%), anemia (55.1% vs 55.3%), neutropenia (46.7% vs 47.0%), fatigue (41.1% vs 37.8%), diarrhea (29.4% vs 23.7%), ALT increase (25.5% vs 24.7%), vomiting (25.5% vs 21.9%), asthenia (24.5% vs 25.4%), constipation (23.7% vs 21.1%), neutrophil count decrease (23.7% vs 28.8%), rash (21.8% vs 15.2%), and peripheral neuropathy (19.7% vs 21.1%).
Following surgery, there were far fewer treatment-related AEs noted. Grade 3 to 5 treatment-related AEs were experienced by 5.7% of those receiving pembrolizumab and for 1.9% of those in the placebo group. The most common treatment-related AEs between the pembrolizumab and placebo groups, respectively, were arthralgia (7.9% vs 6.7%), rash (4.9% vs 2.2%), and pruritus (4.2% vs 2.2%).
"The side effects are relatively comparable between the two arms. We haven't really had any completely new safety signals, we do see more rash with pembrolizumab but otherwise there's very little difference between the two groups on average," Schmid said. "Most of the side effects are side effects of chemotherapy. In the phase after surgery, where patients receive placebo alone or pembrolizumab alone, you can see that the rate of toxicity is very low and there's little difference between the two groups."
The FDA has granted a breakthrough therapy designation to pembrolizumab plus neoadjuvant chemotherapy, based on earlier findings for the combination in patients with high-risk, early-stage TNBC from the KEYNOTE-173 and the I-SPY 2 trials. Submission of a supplemental new drug application for pembrolizumab in TNBC is highly likely, based on the KEYNOTE-522 data.
Reference
Schmid P, Cortes J, Dent R, et al. KEYNOTE-522: Phase 3 study of pembrolizumab + chemotherapy vs placebo + chemotherapy as neoadjuvant treatment, followed by pembrolizumab vs placebo as adjuvant treatment for early-stage high-risk triple-negative breast cancer. Presented at: ESMO Congress 2019, Barcelona, Spain, September 27 to October 1, 2019. Abstract LBA8_PR.
Newsletter
Stay informed on drug updates, treatment guidelines, and pharmacy practice trends—subscribe to Pharmacy Times for weekly clinical insights.
Related Articles
 IMS 2025: Improving Outcomes with Bispecifics in Multiple Myeloma
IMS 2025: Improving Outcomes with Bispecifics in Multiple MyelomaSeptember 19th 2025
 Effectively Managing Immunizations in the Long-Term Care Setting
Effectively Managing Immunizations in the Long-Term Care SettingSeptember 18th 2025