Publication
Article
Pharmacy Practice in Focus: Oncology
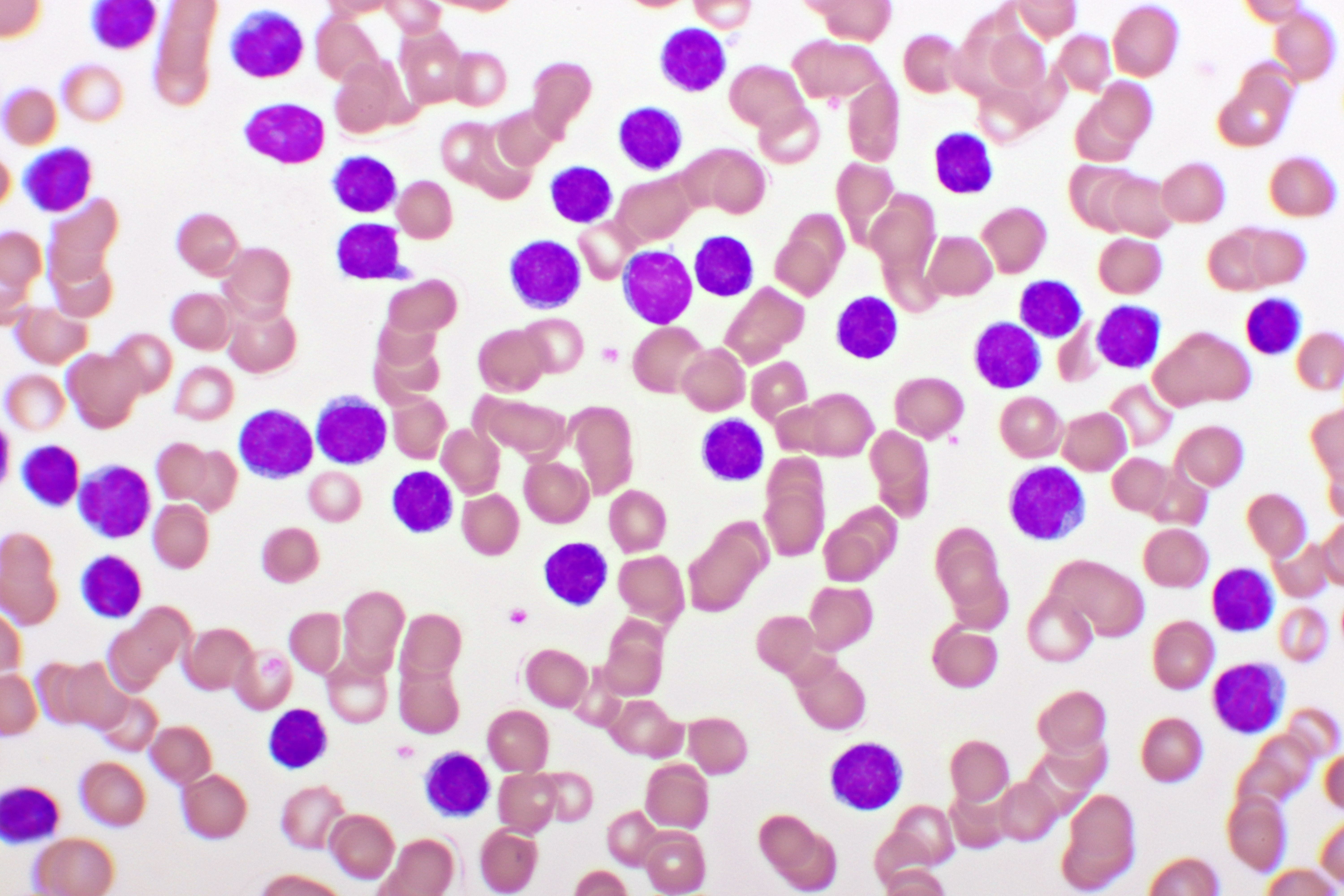
Ibrutinib Plus Venetoclax With MRD-Directed Duration of Treatment Is a New Standard-of-Care Regimen for Previously Unmanaged CLL
Author(s):
The MRD-guided treatment approach has a significant advantage over chemotherapy.
ImaData from the phase 3 FLAIR trial (ISRCTN01844152) showed that the Bruton tyrosine kinase inhibitor ibrutinib (Imbruvica; Pharmacyclics, Janssen Biotech) plus the BCL2 inhibitor venetoclax (Venclexta; AbbVie, Genentech) significantly improved progression-free survival (PFS) and overall survival (OS) compared with the chemotherapy regimen of FCR (fludarabine, cyclophosphamide, rituximab [Rituxan; Genentech]) in unmanaged chronic lymphocytic leukemia (CLL), according to study investigator Peter Hillmen, MBChB, PhD, during a presentation at the 65th American Society of Hematology Annual Meeting & Exposition in San Diego, California. Hillmen, professor of experimental hematology at the University of Leeds in the United Kingdom (UK) and honorary consultant hematologist at Leeds Teaching Hospitals National Health Service Trust, explained that using measurable residual disease (MRD) to direct the duration of ibrutinib plus venetoclax was shown to maximize the outcome of the treatment, with 97.2% PFS at 3 years compared with 76.8% PFS for patients given FCR.1,2
Image credit: jarun011 | stock.adobe.com
During the multicenter, randomized, controlled, open, parallel group FLAIR trial (ISRCTN01844152), investigators recruited patients from 96 centers in the UK between July 20, 2017, and March 24, 2021. Due to the duration period, Hillmen noted that the COVID-19 pandemic had an impact on the trial.1 “This was during the pandemic, so all these assessments were somewhat hampered by the pandemic,” Hillmen said during the presentation.1
The primary end point during the trial was investigator-assessed PFS, and key secondary end points were OS, International Workshop on Chronic Lymphocytic Leukemia response, MRD, and safety. Additionally, end points were analyzed by CLL prognostic subgroups as appropriate.1,2
Investigators enrolled a total of 523 patients with CLL. Included patients had to be fit for treatment with FCR and have no significant comorbidities that would preclude FCR treatment, Hillmen explained. For this reason, patients with more than 20% of cells with 17p deletion were excluded. Among participants, 71.3% were male, median age was 62 years (31.2% > 65 years), and 40.9% were at Binet stage C.1,2
“FCR is given for 6 cycles. This is a conventional schedule that has been used in the UK for 20 years,” Hillmen said. “We can’t give more than 6 cycles, [but we] cannot always give 6 cycles because of cumulative toxicity.”
Patients were randomly assigned to the FCR cohort (n = 263) and ibrutinib plus venetoclax cohort (n = 260). In the ibrutinib plus venetoclax arm, venetoclax was added with a 4-week dose escalation to 400 mg daily and then ibrutinib plus venetoclax was given for up to 6 years, with the duration of ibrutinib plus venetoclax defined by MRD (< 1 CLL cell/100,000 leukocytes [per flow cytometry]).1,2 “Effectively, patients can have between 2 and 6 years of therapy, depending on the speed of response,” Hillmen said.1
Peripheral blood (PB) MRD was assessed at 12 months and then 6 months; if results were negative, the assessment was repeated at 3 months and 6 months in PB and bone marrow (BM). If all assessments showed MRD negativity, then the duration of ibrutinib plus venetoclax was double the time between start of ibrutinib plus venetoclax and the initial MRD-negative PB results, resulting in a duration between 2 and 6 years.1,2
“We gave 2 months of ibrutinib to our patients, then we escalated venetoclax over a 5-week period, which is conventional for venetoclax, and then we gave the combination,” Hillmen said. “Conventionally, these drugs are either given as monotherapy and are given until disease progression, or in the case of venetoclax, [they’re] given in combination, usually with an antibody, but for an arbitrary fixed duration of treatment, which is the same for all patients. In this trial, we modified the duration of therapy by the response of patients, and that’s key for the results.”1
When it comes to measuring CLL disease, Hillmen explained that although it is possible to measure from 1 in 10 cells down to 1 in 100,000 cells quite reliably, measuring to MRD negativity will still lead to some patients experiencing relapse. Hillmen noted this is because it is not currently possible to measure disease to a low enough level.1
“Through a lot of modeling on chemotherapyantibody times, we defined that we had to get below the line of [establishing MRD negativity] to potentially cure or have a major impact on outcome for patients,” Hillmen said. “The way we did this in FLAIR with the ibrutinib plus venetoclax arm was we gave treatment for twice as long as it took to [achieve a] negative [result]. The theory was that the rate of decline would continue at the same rate and we [could] get all patients down to a level that we thought would have a major impact on outcomes.”1
At 2 years of treatment with ibrutinib plus venetoclax, 111 patients (42.7%) stopped the regimen according to the MRD stopping rules. At 3 years, 135 patients (58.1%) stopped treatment according to these rules.1,2
At a median of 43.7 months, Hillmen noted that there were 87 progressions, with 75 in the FCR arm and 12 in the ibrutinib plus venetoclax arm. The HR for PFS for ibrutinib plus venetoclax vs FCR was 0.13 (95% CI, 0.07-0.24; P < .0001), which was consistent for gender, age, or stage. At 3 years, 2.8% of patients had experienced disease progression on ibrutinib plus venetoclax compared with 23.2% on FCR, according to the MRD stopping rules.1,2
There were 34 deaths (25 in the FCR arm and 9 in the ibrutinib plus venetoclax arm), resulting in improved OS for ibrutinib plus venetoclax vs FCR (HR, 0.31; 95% CI, 0.15-0.67; P = .0029). At 3 years, 2% of patients on ibrutinib plus venetoclax had died compared with 7% in the FCR arm. At 9 months (3 months post FCR), 48.3% of patients on FCR attained BM MRD negativity compared with 41.5% taking ibrutinib plus venetoclax. However, with continued treatment on ibrutinib plus venetoclax, more patients were shown to achieve MRD negativity, with the OR of MRD negativity at any time for ibrutinib plus venetoclax vs FCR at 2.03 in BM (95% CI, 1.43-2.89; P < .001) and 3.91 in PB (95% CI, 2.55-6.00; P < .001). Additionally, 90.6% of patients reached MRD negativity in PB at up to 5 years in the ibrutinib plus venetoclax arm, whereas 88% of these patients had MRD negativity in BM at 6 months after their first PB MRD–negative result.1,2
“This is the first time that the combination of these drugs has shown an OS advantage against chemotherapy,” Hillmen said. “Previously, PFS has been shown to have an advantage in the [clinical trials that used] time-limited treatments.”1
In the prognostic subgroups included in the trial, 56.9% of patients had immunoglobulin heavy-chain variable region gene (IGHV)–unmutated (≥ 98% homology to germline) disease, 37.6% had IGHV-mutated disease, and 5.5% had subset 2 disease.2 When looking at results among the prognostic subgroups, Hillmen noted that investigators saw an OS advantage among the IGHV-unmutated disease subgroup, which included approximately half of the patients in the trial. In the IGHV-mutated disease subgroup, there was no significant difference in PFS or OS or the HR was in favor of the combination approach guided by MRD, according to Hillmen.1
“The combination is well tolerated, [although] there are still expected toxicities with both venetoclax and ibrutinib,” Hillmen said.1 Specifically, serious adverse events (SAEs) were reported in 252 patients (51.3%; 129 who received FCR vs 123 who received ibrutinib plus venetoclax). Notable SAEs by organ class were infections in 18.8% of patients who received FCR vs 22.2% who received ibrutinib plus venetoclax, blood and lymphatic SAEs in 31% vs 5%, and cardiac SAEs in 0.4% vs 10.7%, respectively.1,2
Furthermore, 4 patients had sudden or cardiac deaths, which were evenly split in both arms, with 2 in the FCR arm and 2 in the ibrutinib plus venetoclax arm. Additionally, 69 other cancers were diagnosed (45 in the FCR arm, 24 in the ibrutinib plus venetoclax arm) in 51 patients (34 in the FCR arm, 17 in the ibrutinib plus venetoclax arm) during the trial. The incidence of other cancers per 100 patient-years was also greater for FCR vs ibrutinib plus venetoclax at 5.4 (95% CI, 5.11-5.68) vs 2.6 (95% CI, 2.40-2.79), respectively. Of the additional cancers that arose, there were 7 cases of myelodysplastic syndromes (MDS) or acute myeloid leukemia (AML) in the FCR arm and 1 in the ibrutinib plus venetoclax arm.1,2
“Occurrence of MDS and AML is often a fatal complication of chemotherapy treatments, and that’s a significant difference,” Hillmen said. “This is the first trial [with results] to show that the MRD-guided approach with treatment beyond negativity has a significant advantage over chemotherapy, both in terms of PFS and OS. Over 90% of patients achieved MRD-negative remission with this combination in PB, which hadn’t been seen in other trials. This is seen across all subgroups apart from the patients [with] IGHV-mutated [disease], where there’s a trend in favor of ibrutinib plus venetoclax.”1
Additionally, there were no unexpected toxicities or multiple toxicities during the trial. In fact, Hillmen noted that a previous part of the trial showed sudden deaths and cardiac deaths in the ibrutinib plus venetoclax arm, but this was not seen in this part of the trial.1
“This may be because we modified the trial during the trial to be much more aware of cardiac abnormalities and hypertension,” Hillmen said. “The results seen here are better than any other phase 3 trial with targeted treatment in terms of PFS and OS. We have another part of the trial that will probably be coming next year with a third arm, with ibrutinib monotherapy as another control arm.”1
Hillmen also explained that since the pandemic, FCR has not been used as standard of care for the management of CLL in the UK. Specifically, FCR has been mostly replaced by other combination therapies, such as venetoclax and ibrutinib, because of the toxicities associated with FCR.1,2
“I think the big issue for targeted [management] for CLL is the duration of therapy, which can be very long in the front line and is associated with toxicity and potential resistance,” Hillmen said. “So we [work to] give time-limited therapy and potentially cure patients with the combinations that we have.”1
References
1. Hillmen P. Is more or less better? reviewing therapies in hematologic cancers. Presented at: 65th American Society of Hematology Annual Meeting & Exposition; December 9-12, 2023; San Diego, CA.
2. Hillmen P, Cairns DA, Bloor AJC, et al. Ibrutinib plus venetoclax with MRD-directed duration of treatment is superior to FCR and is a new standard of care for previously untreated CLL: report of the phase III UK NCRI FLAIR study. Abstract presented at: 65th American Society of Hematology Annual Meeting & Exposition; December 9-12, 2023; San Diego, CA. Abstract 631. https://ash.confex.com/ash/2023/webprogram/Paper178298.html
Newsletter
Stay informed on drug updates, treatment guidelines, and pharmacy practice trends—subscribe to Pharmacy Times for weekly clinical insights.





