Publication
Article
Pharmacy Practice in Focus: Oncology
Advancing Treatment Selection in CLL Management
Treatment options are distinct in their mechanisms, safety profiles, and implications for patients’ quality of life.
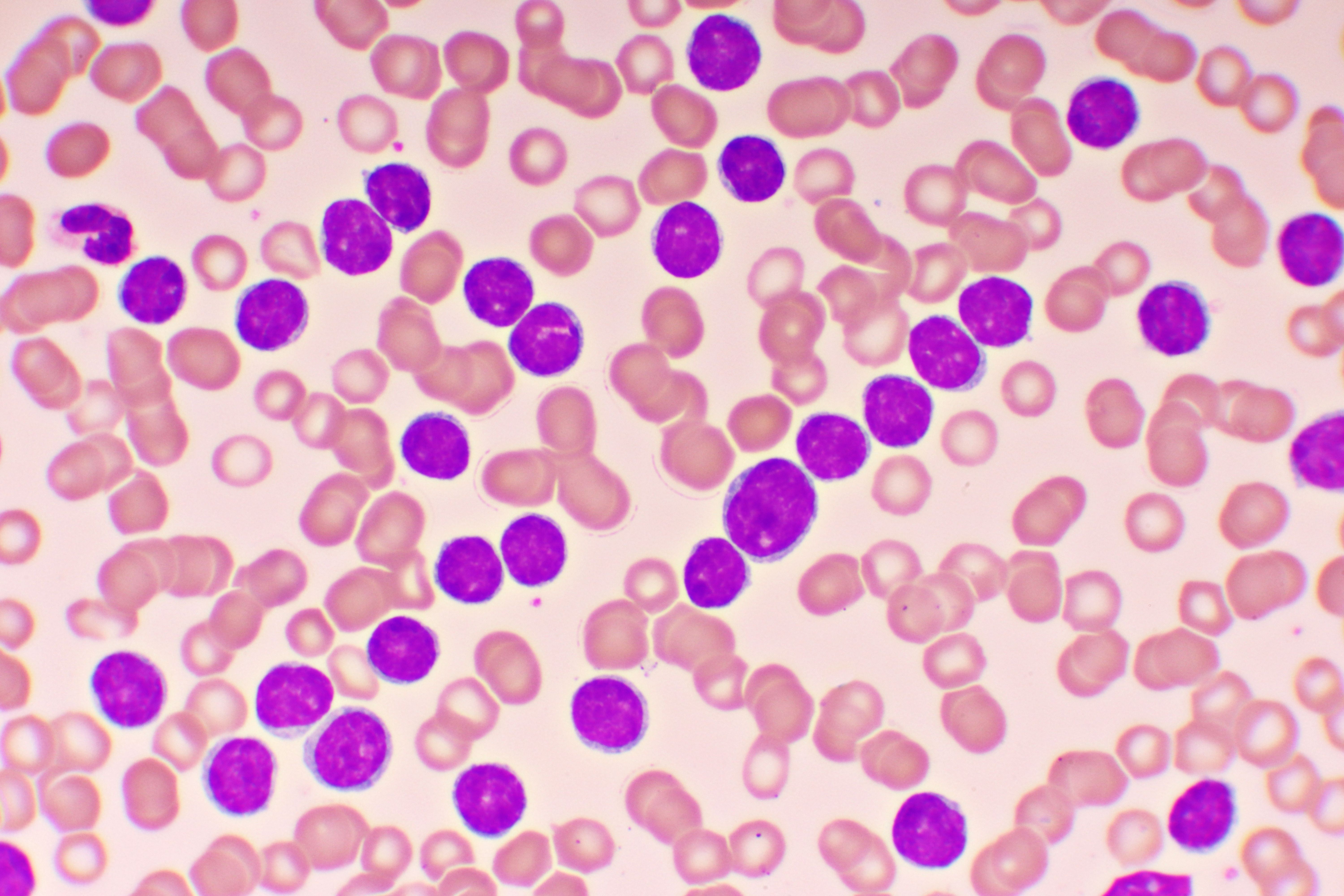
Chronic lymphocytic leukemia (CLL) is a mature B-cell neoplasm distinguished by the progressive accumulation of monoclonal B lymphocytes.1 It remains the most common type of adult leukemia in Western countries, with an estimated 18,740 new cases projected for 2023, underscoring its prevalence as the foremost form of chronic leukemia in the United States. CLL primarily affects older adults, with 69 years being the median age of diagnosis.1,2 Notably, approximately 35% of CLL cases are diagnosed in individuals younger than 65 years, reflecting a broader age range than previously recognized. The 5-year relative survival rate for CLL has made significant advances; from 66.2% in 1975, it has risen to an estimated 87.7% in 2019, which may be attributed to recent progress in treatment options.2
Image credit: jarun011 | stock.adobe.com
The clinical presentation and progression of CLL can vary widely. Approximately 30% of patients may exhibit an asymptomatic, indolent course that necessitates no intervention. In contrast, others may experience active disease characterized by progressive lymphocytosis, cytopenias, lymphadenopathy, hepatosplenomegaly, and B symptoms such as weight loss, night sweats, and fever.1
CLL is characterized by the clonal proliferation of mature CD5+ B cells, infiltrating the blood and secondary lymphoid organs, with impaired apoptosis as a result of oncogene overexpression (ie, BCL2).1,3 The pathogenesis of CLL often begins with the gain or loss of large chromosomal material; nearly 80% of patients with CLL harbor at least 1 of the 4 common chromosomal alterations: del(13q), del(11q), del(17p), or trisomy 12.4,5 Specifically, deletions frequently affect band 17p13, the locus of the crucial tumor suppressor gene TP53. Mutations in TP53, which occur in 4% to 37% of CLL cases, have been consistently associated with a very poor prognosis.6,7
Other pathogenetic drivers are implicated in B-cell–receptor (BCR) signaling. Bruton tyrosine kinase (BTK), belonging to the Tec family of protein tyrosine kinases, stands out as a crucial component for activating several pathways that are constitutively active and essential for CLL cell survival. Similarly, phosphatidylinositol 3-kinase (PI3K)–δ, a lipid kinase instrumental in normal B-cell development and function, and in signal transduction from receptors, is notably hyperactive in CLL.1,8 For the diagnosis of CLL, a critical threshold of lymphocytosis (> 5000 cells/mm3) is identified, along with a characteristic immunophenotype via flow cytometry.1
The Rai and Binet staging systems remain central to stratifying patients with CLL into prognostic groups that correlate with distinct clinical outcomes.9,10 Both staging systems are instrumental in determining the initiation of treatment. For patients presenting with asymptomatic, low-risk CLL, as defined by Rai stage 0 or Binet stage A, or those with intermediate-risk CLL (Rai stage I-II or Binet stage B), a watch-and-wait strategy is typically adopted. This approach is substantiated by clinical data indicating no significant overall survival (OS) advantage with early intervention in these stages.11
When it comes to therapeutic commencement, the International Workshop on Chronic Lymphocytic Leukemia guidelines recommend considering factors beyond the Rai and Binet stages. Indications for initiating treatment include the presence of severe B symptoms, such as significant weight loss, night sweats, and fevers, or any signs indicative of endangered end-organ function. Other criteria include pronounced splenomegaly or lymphadenopathy and progressive or steroid-refractory autoimmune cytopenias.12 The criteria aim is to ensure that treatment is reserved for patients who will most likely benefit from it, thereby avoiding unnecessary early intervention for those with indolent disease courses.
Historically, chemoimmunotherapies (CITs) such as chlorambucil (Leukeran; Excella GmbH & Co) plus obinutuzumab (GClb; Gazyva, Genentech USA), bendamustine plus rituximab (BR; Rituxan, Genentech USA), and fludarabine plus cyclophosphamide plus rituximab (FCR) were recommended first-line therapies for CLL without del(17p)/TP53 mutation, but recently their use has been relegated in the National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology (NCCN Guidelines) version 1.2024. These regimens are now considered primarily when BTK inhibitors and venetoclax (Venclexta; AbbVie, Genentech USA) are unavailable or contraindicated, or when rapid disease debulking is required.13 Instead, BTK inhibitor– or venetoclax-based regimens are now the preferred first-line therapies in CLL with or without del(17p)/TP53 mutation.13 This shift was backed up by the comparatively limited benefit in progression-free survival (PFS) provided by CITs when contrasted with small-molecule inhibitors, despite similar OS rates.14-18 The ELEVATE-TN study (NCT02475681) demonstrated a 48-month PFS of 87% for acalabrutinib (Calquence; AstraZeneca) plus obinutuzumab compared with 25% for GClb.14 The iLLUMINATE study (NCT02264574) showed a 30-month PFS of 79% for ibrutinib (Imbruvica; Pharmacyclics) plus obinutuzumab vs 31% for GClb.15 One study by the Alliance for Clinical Trials in Oncology (NCT01886872) reported a 4-year PFS of 76% for the ibrutinib plus rituximab cohort vs 47% for BR.16 Zanubrutinib (Brukinsa; BeiGene) also exhibited a superior PFS rate (86% vs. 70% for BR; HR, 0.42; P < .0001).17 Moreover, the CLL14 trial (NCT02242942) revealed a 3-year PFS of 82% for the combination of venetoclax plus obinutuzumab, compared with 50% for GClb (HR, 0.31; P < .0001).18 These significant improvements in PFS highlighted the impact of BTK inhibitor– or venetoclax-based regimens on the management of CLL, supporting their prioritization in treatment lines.
Both BTK inhibitors and BCL-2 inhibitors are highly efficacious, yielding an overall response rate (ORR) in excess of 90%.14,17-24 The critical question arises: Between these 2 prominent drug classes, which should be the initial choice of therapy? The NCCN guidelines provide a broad framework, leaving significant discretion in the decision-making process, given the paucity of prospective clinical trials directly comparing the efficacy of BTK inhibitors to venetoclax as initial treatments in patients with CLL.13
Venetoclax, an oral selective small-molecule inhibitor of BCL-2, targets the antiapoptotic protein overexpressed in CLL cells—a factor implicated in tumor cell survival and treatment resistance.1,19 The binding of venetoclax to BCL-2 reinstates the apoptotic process. Its efficacy, in combination with obinutuzumab, in treating CLL was substantiated by the CLL14 study, which demonstrated significantly improved PFS after 40 months of follow-up (HR, 0.31; P < .0001).18
The VenG regimen (12 cycles of venetoclax and 6 cycles of obinutuzumab), leveraging synergistic mechanisms for enhanced remission durability, presents a financially prudent nonchemotherapy alternative to the indefinite treatment duration typically associated with BTK inhibitors.18 This fixed-term approach may be particularly advantageous for patients facing financial constraints. Additionally, it presents a viable option for patients with specific chronic comorbidities, especially hypertension, atrial fibrillation, or chronic heart failure, and those on warfarin or with hemophilia, as it is less likely to exacerbate these conditions, unlike BTK inhibitors. In spite of these advantages, patients must be apprised of the 5-week dosing for venetoclax (to minimize the risk of developing tumor lysis syndrome [TLS]) and the complicated dosing schedule for obinutuzumab, which requires more frequent clinic visits and intravenous administration. Shared decision-making is vital in discussing these aspects.18,19,22
Moreover, venetoclax has shown efficacy in managing relapsed or refractory CLL (R/R CLL) post ibrutinib treatment. Several retrospective analyses indicated that venetoclax treatment correlated with favorable ORR and PFS in patients who have previously experienced ibrutinib failure.25-27 It is important to note, however, that the presence of a TP53 mutation is associated with a significantly increased risk of relapse (HR, 1.7; 95% CI, 1.2-2.4) during this fixed-duration therapy.28
As mentioned, an important consideration when using venetoclax is the risk of TLS, despite the generally low occurrence (approximately 1%) across major clinical trials if patients are equipped with adequate prophylaxis.18,20 The regimen’s demand for intensive hydration to prevent TLS may not be suitable for patients with limited cardiac and/or renal function, where volume overload might be a concern. Vigilant monitoring is critical for patients with predisposing factors like bulky lymph nodes, renal injury, existing leukocytosis, hyperuricemia, or electrolyte imbalances.13
Drug-drug interactions present another challenge with venetoclax-based treatments. As a major substrate of CYP3A4, venetoclax levels can be significantly affected by potent CYP3A4 inhibitors, such as certain antifungals in the azole class, leading to contraindications during initiation and the ramp-up phase for patients with CLL, as well as a 2- to 3-day washout after inhibitor discontinuation. Patients should be counseled on the consumption of grapefruit products, Seville oranges, and star fruit, as they should avoid these products due to similar interaction risks. Venetoclax can also raise warfarin levels, increasing bleeding risk and necessitating more frequent international normalized ratio monitoring. Moreover, it can affect the levels of P-glycoprotein substrates, which should be dosed at least 6 hours prior to venetoclax administration.19,21
BTK inhibitors, including ibrutinib from the first generation (nonselective), as well as acalabrutinib and zanubrutinib from the second generation (selective), are oral small molecules impeding Bruton tyrosine kinase, integral to the BCR and cytokine receptor signaling pathways, through covalent binding to the C481 residue. By modulating BTK activity, these inhibitors downregulate B-cell proliferation, trafficking, chemotaxis, and adhesion, leading to diminished proliferation and increased apoptosis of malignant B cells, as well as redistribution lymphocytosis (at the beginning of therapy).23
Durable responses to BTK inhibitors have been commendable. The RESONATE-2 study (NCT01722487), featuring up to 7 years of follow-up, highlighted a substantial and enduring PFS advantage in patients receiving ibrutinib over chlorambucil (HR, 0.160; 95% CI, 0.111-0.230). Specifically, a PFS of 61% was reported for ibrutinib at 6.5 years compared with just 9% for chlorambucil. This improvement spanned all patient subgroups, even those with high-risk genetic profiles such as unmutated IGHV or del(11q).24 In major clinical trials showing better PFS, ibrutinib was given continuously until disease progression, with or without other fixed-duration add-ons like anti-CD20 monoclonal antibodies, implying continuous and indefinite treatment may contribute to the extended survival in patients with higher-risk disease profiles.15,16,29
The ease of administration is a notable advantage of BTK inhibitors; flat-dose tablets are used without the need for additional clinic visits for dose escalation or titration.23,30-32 Nevertheless, long-term use of BTK inhibitors could be limited by certain adverse effects (AEs) commonly seen in patients taking ibrutinib.
Bleeding complications stand as a significant concern with BTK inhibitors, attributed to the role of BTK in collagen-mediated platelet activation. Impairment of BTK disrupts platelet adhesion to von Willebrand factor-coated surfaces, leading to coagulation issues.33 Clinical trials underscore this risk, with reported bleeding events being substantial across the major phase 3 trials: 51% in the ELEVATE-RR study (NCT02477696) for ibrutinib; 38% in the ELEVATE-RR study for acalabrutinib; and 45% in the SEQUOIA study (NCT03336333) for zanubrutinib.34,35 The disparate incidence rates among these inhibitors may be influenced by off-target effects on Tec kinase—ibrutinib and zanubrutinib, unlike acalabrutinib, inhibit Tec, potentially contributing to higher bleeding rates.36 Specifically, ibrutinib’s pronounced effect could be due to its additional suppression of platelet surface receptors (GPIbα, GPIX, and integrin αIIbβ3), alongside Tec inhibition.37
In considering cardiovascular toxicities, it is noteworthy that all BTK inhibitors are associated with an elevated risk of atrial fibrillation and hypertension due to their blockade of ErbB4/HER4, a kinase integral to cardiac conduction.38 This risk, notwithstanding, is not uniformly distributed among the BTK inhibitors. For instance, in the ELEVATE-RR study, acalabrutinib demonstrated a significantly lower incidence of all-grade atrial fibrillation/atrial flutter compared with ibrutinib (9.4% vs 16.0%; P = .02). A similar trend was observed in the ALPINE study (NCT03734016), with zanubrutinib exhibiting a 5.2% incidence rate compared with ibrutinib’s 13.3%.39 The unique ability of ibrutinib to bind simultaneously to ErbB2/HER2 and ErbB4/HER4, leading to downstream inhibition of cardiac PI3K-AKT, may explain its higher incidence of cardiac arrhythmias.32
Diarrhea and arthralgia are also recognized AEs linked to BTK inhibitors, and while the exact mechanism is not entirely understood, they may be attributed to off-target EGFR inhibition.33 These AEs appear with comparable frequency across the class of BTK inhibitors, manifesting in approximately 40% to 50% of cases for diarrhea and 15% to 25% for arthralgia, respectively.34,35 Acalabrutinib, in particular, has been associated with a higher incidence of headache compared with ibrutinib (35% vs 20% in the ELEVATE-RR study), which is usually transient for a few weeks and can be mitigated with supportive measures such as acetaminophen and caffeine.34
Neutropenia and infections are also prevalent with BTK inhibitor therapy. Zanubrutinib was noted for a higher neutropenia rate (28% in the ALPINE study vs 22% for ibrutinib) while showing comparable infection rates (60% vs 63%).39 Acalabrutinib led to neutropenia in 12% of patients and infections in 74% within the ELEVATE-TN study.14 Consequently, antimicrobial prophylaxis against Pneumocystis jirovecii pneumonia and varicella-zoster virus is generally recommended, alongside monitoring for fungal infections.13 Similar to venetoclax, all BTK inhibitors are major substrates of CYP3A4, requiring heightened vigilance and meticulous monitoring when patients are concurrently administered CYP3A4 inhibitors.23,30,31
Given the safety profiles of the BTK inhibitors, it is reasonable to consider alternatives to BTK inhibitors for patients with significant cardiovascular conditions, such as unmanageable atrial fibrillation or hypertension, bleeding disorders (eg, hemophilia), or requiring anticoagulation therapy with warfarin. Acalabrutinib and zanubrutinib were shown to be effective for the management of patients with ibrutinib intolerance, attributable to their narrower off-target activity and a more favorable safety profile.13 An in vitro study indicated that acalabrutinib exhibits even fewer off-target effects beyond BTK inhibition, which may correlate with the slightly improved AE profile observed in terms of bleeding, hypertension, and grade 3 AEs.33 This was supported by a matching-adjusted indirect comparison (MAIC) of phase 3 trial data for acalabrutinib (from the ASCEND study [NCT05042128]) and zanubrutinib (from the ALPINE study) presented at the 2023 American Society of Clinical Oncology Annual Meeting.40
In the realm of R/R CLL, second-generation BTK inhibitors have shown promising efficacy. The ELEVATE-RR study, with a median follow-up duration of 40.9 months, established acalabrutinib as noninferior to ibrutinib, demonstrating a median PFS of 38.4 months (HR, 1.00; 95% CI, 0.79-1.27), while in the ALPINE study, with a median follow-up of 29.6 months, zanubrutinib showed a superior PFS compared with ibrutinib (87 vs 118 occurrences of disease progression or death; HR, 0.65; 95% CI, 0.49-0.86; P = .002).34,39
Although these 2 studies had different objectives (noninferiority vs superiority), the MAIC of the ASCEND and ALPINE studies indicated comparable PFS between acalabrutinib and zanubrutinib (HR, 0.90; 95% CI; 0.60-1.36).41 Further head-to-head study is necessary to test this hypothesis.
The presence of BTK C481 mutations, detected in about 69% of patients with disease relapse approximately 12 months prior to clinical relapse in the context of acalabrutinib treatment, is a significant mechanism of resistance to covalent BTK inhibitors due to their interaction with the C481 residue.13,41,42 Pirtobrutinib (Jaypirca; Eli Lilly and Company) emerges as a counteractive strategy, being a selective, noncovalent (reversible) BTK inhibitor that targets both wild-type and C481-mutant BTK with similar low nanomolar potency.33 This design aims to circumvent the resistance challenges posed by covalent BTK inhibitors.43 The BRUIN study (NCT03740529) showcased encouraging outcomes for pirtobrutinib, where subjects previously treated with at least 1 BTK inhibitor demonstrated an ORR of 73.3% (95% CI, 67.3-78.7) and a median PFS of 19.6 months (95% CI, 16.9-22.1) over a median follow-up of 19.4 months, with around 40% of these patients having also received venetoclax treatment.44
These promising results have influenced the NCCN Guidelines to recognize pirtobrutinib as a category 2A recommendation for patients with resistance or intolerance to prior covalent BTK inhibitors, applicable as a second- or third-line treatment for CLL despite its current off-label status.13
As we navigate the evolving landscape of CLL therapeutics, it is imperative to acknowledge that while the treatment options at our disposal are robustly effective, they are distinct in their mechanisms, safety profiles, and implications or patients’ quality of life. In crafting a patient-centered regimen, the convergence of expertise from physicians and pharmacists, paired with the values and preferences of patients, becomes paramount. This collaborative approach ensures that shared decision-making is not just a guiding principle but a practiced reality, empowering each patient with a tailored strategy that optimally aligns with their unique clinical circumstances. The future of CLL management lies in this synergistic partnership, which promises not only improved clinical outcomes but also the holistic well-being of those we serve.
References
- Burger JA. Treatment of chronic lymphocytic leukemia. N Engl J Med. 2020;383(5):460-473. doi:10.1056/NEJMra1908213
- Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2023;73(1):17-48. doi:10.3322/caac.21763
- Hallek M, Cheson BD, Catovsky D, et al. iwCLL guidelines for diagnosis, indications for treatment, response assessment, and supportive management of CLL. Blood. 2018;131(25):2745-2760. doi:10.1182/blood-2017-09-806398
- Landau DA, Tausch E, Taylor-Weiner AN, et al. Mutations driving CLL and their evolution in progression and relapse. Nature. 2015;526(7574):525-530. doi:10.1038/nature15395
- Döhner H, Stilgenbauer S, Benner A, et al. Genomic aberrations and survival in chronic lymphocytic leukemia. N Engl J Med. 2000;343(26):1910-1916. doi:10.1056/NEJM200012283432602
- Hallek M, Fischer K, Fingerle-Rowson G, et al. Addition of rituximab to fludarabine and cyclophosphamide in patients with chronic lymphocytic leukaemia: a randomised, open-label, phase 3 trial. Lancet. 2010;376(9747):1164-1174. doi:10.1016/S0140-6736(10)61381-5
- Zenz T, Vollmer D, Trbusek M, et al. TP53 mutation profile in chronic lymphocytic leukemia: evidence for a disease specific profile from a comprehensive analysis of 268 mutations. Leukemia. 2010;24(12):2072-2079. doi:10.1038/leu.2010.208
- Hallek M. Chronic lymphocytic leukemia: 2020 update on diagnosis, risk stratification and treatment. Am J Hematol. 2019;94(11):1266-1287. doi:10.1002/ajh.25595
- Rai KR, Sawitsky A, Cronkite EP, Chanana AD, Levy RN, Pasternack BS. Clinical staging of chronic lymphocytic leukemia. Blood. 1975;46(2):219-234. Blood. 2016;128(17):2109. doi:10.1182/blood-2016-08-737650
- Binet JL, Auquier A, Dighiero G, et al. A new prognostic classification of chronic lymphocytic leukemia derived from a multivariate survival analysis. Cancer. 1981;48(1):198-206. doi:10.1002/1097-0142(19810701)48:1<198::aid-cncr2820480131>3.0.co;2-v.
- Herling CD, Cymbalista F, Groß-Ophoff-Müller C, et al. Early treatment with FCR versus watch and wait in patients with stage Binet A high-risk chronic lymphocytic leukemia (CLL): a randomized phase 3 trial. Leukemia. 2020;34(8):2038-2050. doi:10.1038/s41375-020-0747-7
- Hallek M, Cheson BD, Catovsky D, et al. iwCLL guidelines for diagnosis, indications for treatment, response assessment, and supportive management of CLL. Blood. 2018;131(25):2745-2760. doi:10.1182/blood-2017-09-806398
- NCCN. Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Chronic Lymphocytic Leukemia/ Small Lymphocytic Lymphoma Version 1.2024. NCCN. November 3, 2023. Accessed November 6, 2023. https://www.nccn.org/professionals/physician_gls/pdf/cll.pdf
- Sharman JP, Egyed M, Jurczak W, et al. Efficacy and safety in a 4-year follow-up of the ELEVATE-TN study comparing acalabrutinib with or without obinutuzumab versus obinutuzumab plus chlorambucil in treatment-naïve chronic lymphocytic leukemia. Leukemia. 2022;36(4):1171-1175. doi:10.1038/s41375-021-01485-x
- Moreno C, Greil R, Demirkan F, et al. Ibrutinib plus obinutuzumab versus chlorambucil plus obinutuzumab in first-line treatment of chronic lymphocytic leukaemia (iLLUMINATE): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20(1):43-56. doi:10.1016/S1470-2045(18)30788-5
- Woyach JA, Ruppert AS, Heerema NA, et al. Long-term results of Alliance A041202 show continued advantage of ibrutinib-based regimens compared with bendamustine plus rituximab (BR) chemoimmunotherapy. Blood. 2021;138(suppl 1):639-639. doi:10.1182/blood-2021-153146
- Tam CS, Giannopoulos K, Jurczak W, et al. Sequoia: Results of a phase 3 randomized study of zanubrutinib versus bendamustine + rituximab (BR) in patients with treatment-naïve (TN) chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL). Blood. 2021;138(suppl 1):396. doi:10.1182/blood-2021-148457
- Al-Sawaf O, Zhang C, Tandon M, et al. Venetoclax plus obinutuzumab versus chlorambucil plus obinutuzumab for previously untreated chronic lymphocytic leukaemia (CLL14): follow-up results from a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2020;21(9):1188-1200. doi:10.1016/S1470-2045(20)30443-5
- Venclexta. Prescribing information. AbbVie, Inc; 2022. Accessed January 9, 2024. https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/208573s027lbl.pdf
- Roberts AW, Davids MS, Pagel JM, et al. Targeting BCL2 with venetoclax in relapsed chronic lymphocytic leukemia. N Engl J Med. 2016;374(4):311-322. doi:10.1056/NEJMoa1513257
- Venetoclax. Lexi-Drugs. Hudson, OH: Lexicomp, 2023. Updated November 1, 2023. Accessed November 7, 2023. https://online.lexi.com/lco/action/login
- Gazyva. Prescribing information. Genentech, Inc; 2017. Accessed November 7, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/125486s017s018lbl.pdf
- Imbruvica. Prescribing information. Pharmacyclics, LLC; 2022. Accessed November 7, 2023.
- Barr PM, Owen C, Robak T, et al. Up to seven years of follow-up in the resonate-2 study of first-line IBRUTINIB treatment for patients with chronic lymphocytic leukemia. J Clin Oncol. 2021;39(suppl 15):7523. doi:10.1200/jco.2021.39.15_suppl.7523
- Jones JA, Mato AR, Wierda WG, et al. Venetoclax for chronic lymphocytic leukaemia progressing after ibrutinib: an interim analysis of a multicentre, open-label, phase 2 trial. Lancet Oncol. 2018;19(1):65-75. doi:10.1016/S1470-2045(17)30909-9
- Eyre TA, Kirkwood AA, Gohill S, et al. Efficacy of venetoclax monotherapy in patients with relapsed chronic lymphocytic leukaemia in the post-BCR inhibitor setting: a UK wide analysis. Br J Haematol. 2019;185(4):656-669. doi:10.1111/bjh.15802
- Innocenti I, Morelli F, Autore F, et al. Venetoclax in CLL patients who progress after B-cell receptor inhibitor treatment: a retrospective multi-centre Italian experience. Br J Haematol. 2019;187(1):e8-e11. doi:10.1111/bjh.16123
- Roberts AW, Ma S, Kipps TJ, et al. Efficacy of venetoclax in relapsed chronic lymphocytic leukemia is influenced by disease and response variables. Blood. 2019;134(2):111-122. doi:10.1182/blood.2018882555
- Burger JA, Sivina M, Jain N, et al. Randomized trial of ibrutinib vs ibrutinib plus rituximab in patients with chronic lymphocytic leukemia. Blood. 2019;133(10):1011-1019. doi:10.1182/blood-2018-10-879429
- Calquence. Prescribing information. AstraZeneca Pharmaceuticals LP; 2022. Accessed November 7, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/216387Orig2s000Correctedlbl.pdf
- Brukinsa. Prescribing information. BeiGene, Ltd; 2023. Accessed November 7, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/213217s007lbl.pdf
- Jaypirca. Prescribing information. Lilly USA, LLC; 2023. Accessed November 7, 2023. https://pi.lilly.com/us/jaypirca-uspi.pdf
- Estupiñán HY, Berglöf A, Zain R, Smith CIE. Comparative analysis of BTK inhibitors and mechanisms underlying adverse effects. Front Cell Dev Biol. 2021;9:630942. doi:10.3389/fcell.2021.630942
- Byrd JC, Hillmen P, Ghia P, et al. Acalabrutinib versus ibrutinib in previously treated chronic lymphocytic leukemia: results of the first randomized phase III trial. J Clin Oncol. 2021;39(31):3441-3452. doi:10.1200/JCO.21.01210
- Tam CS, Robak T, Ghia P, et al. Zanubrutinib monotherapy for patients with treatment naïve chronic lymphocytic leukemia and 17p deletion. Haematologica. 2020;106(9):2354-2363. doi:10.3324/haematol.2020.259432
- Nicolson PLR, Hughes CE, Watson S, et al. Inhibition of Btk by Btk-specific concentrations of ibrutinib and acalabrutinib delays but does not block platelet aggregation mediated by glycoprotein VI. Haematologica. 2018;103(12):2097-2108. doi:10.3324/haematol.2018.193391
- Dobie G, Kuriri FA, Omar MMA, et al. Ibrutinib, but not zanubrutinib, induces platelet receptor shedding of GPIb-IX-V complex and integrin αIIbβ3 in mice and humans. Blood Adv. 2019;3(24):4298-4311. doi:10.1182/bloodadvances.2019000640
- Milano GA, Serres E, Ferrero JM, Ciccolini J. Trastuzumab-induced cardiotoxicity: is it a personalized risk?. Curr Drug Targets. 2014;15(13):1200-1204. doi:10.2174/1389450115666141114151911
- Brown JR, Eichhorst B, Hillmen P, et al. Zanubrutinib or ibrutinib in relapsed or refractory chronic lymphocytic leukemia. N Engl J Med. 2023;388(4):319-332. doi:10.1056/NEJMoa2211582
- Ghia P, Pluta A, Wach M, et al. Acalabrutinib versus investigator’s choice in relapsed/refractory chronic lymphocytic leukemia: final ASCEND trial results. Hemasphere. 2022;6(12):e801. doi:10.1097/HS9.0000000000000801
- Kittai AS, Skarbnik, A, Miranda M, et al. A matching-adjusted indirect comparison (MAIC) of the efficacy and safety of acalabrutinib (acala) versus zanubrutinib (zanu) in relapsed or refractory chronic lymphocytic leukemia (RR CLL). Presented at: American Society of Clinical Oncology Annual Meeting; June 2-6, 2023; Chicago, IL. https://meetings.asco.org/abstracts-presentations/220358
- Byrd JC, Jones D, Lozanski G, et al. Resistance to acalabrutinib in CLL is mediated primarily by BTK mutations [abstract]. Blood. 2019;134:Abstract 504. doi:10.1182/blood.2020006783
- Gomez EB, Ebata K, Randeria HS, et al. Preclinical characterization of pirtobrutinib, a highly selective, noncovalent (reversible) BTK inhibitor. Blood. 2023;142(1):62-72. doi:10.1182/blood.2022018674
- Mato AR, Woyach JA, Brown JR, et al. Pirtobrutinib after a covalent BTK inhibitor in chronic lymphocytic leukemia. N Engl J Med. 2023;389(1):33-44. doi:10.1056/NEJMoa2300696
About the Authors
Yijun Cai is a class of 2024 PharmD candidate in the Titus Family Department of Clinical Pharmacy, Alfred E. Mann School of Pharmacy and Pharmaceutical Sciences, University of Southern California (USC), in Los Angeles, and in the Jane Anne Nohl Division of Hematology, Keck School of Medicine of USC in Los Angeles.
Amir Ali, PharmD, BCOP, is a clinical pharmacist specialist and residency program coordinator at USC Norris Comprehensive Cancer Center and adjunct assistant professor of pharmacy practice at the USC Mann School of Pharmacy.
Newsletter
Stay informed on drug updates, treatment guidelines, and pharmacy practice trends—subscribe to Pharmacy Times for weekly clinical insights.

FDA Approves Linvoseltamab-Gcpt for Treatment of Relapsed or Refractory Multiple Myeloma




