News
Article
Unveiling the Microbiota's Role in Cancer: From Tumorigenesis to Treatment
Author(s):
The gut and intratumoral microbiota influence cancer development, progression, and treatment responses, highlighting the potential for treatment strategies that leverage these microbial interactions to enhance cancer therapies.
Gut and intratumoral microbiota play a significant role not only in tumorigenesis but also in shaping responses to cancer treatments, explained Maria Rescigno, PhD, professor and vice rector for research at Humanitas University and deputy scientific director and group leader of the Immunology Program and the Mucosal Immunology and Microbiota Lab at Humanitas Research Hospital in Milan, Italy. During a session at the European Society for Medical Oncology (ESMO) Congress 2024 in Barcelona, Spain, Rescigno explained that understanding these dynamics can pave the way for innovative treatment strategies that leverage the microbiota to improve treatment outcomes.
Gut Microbiota
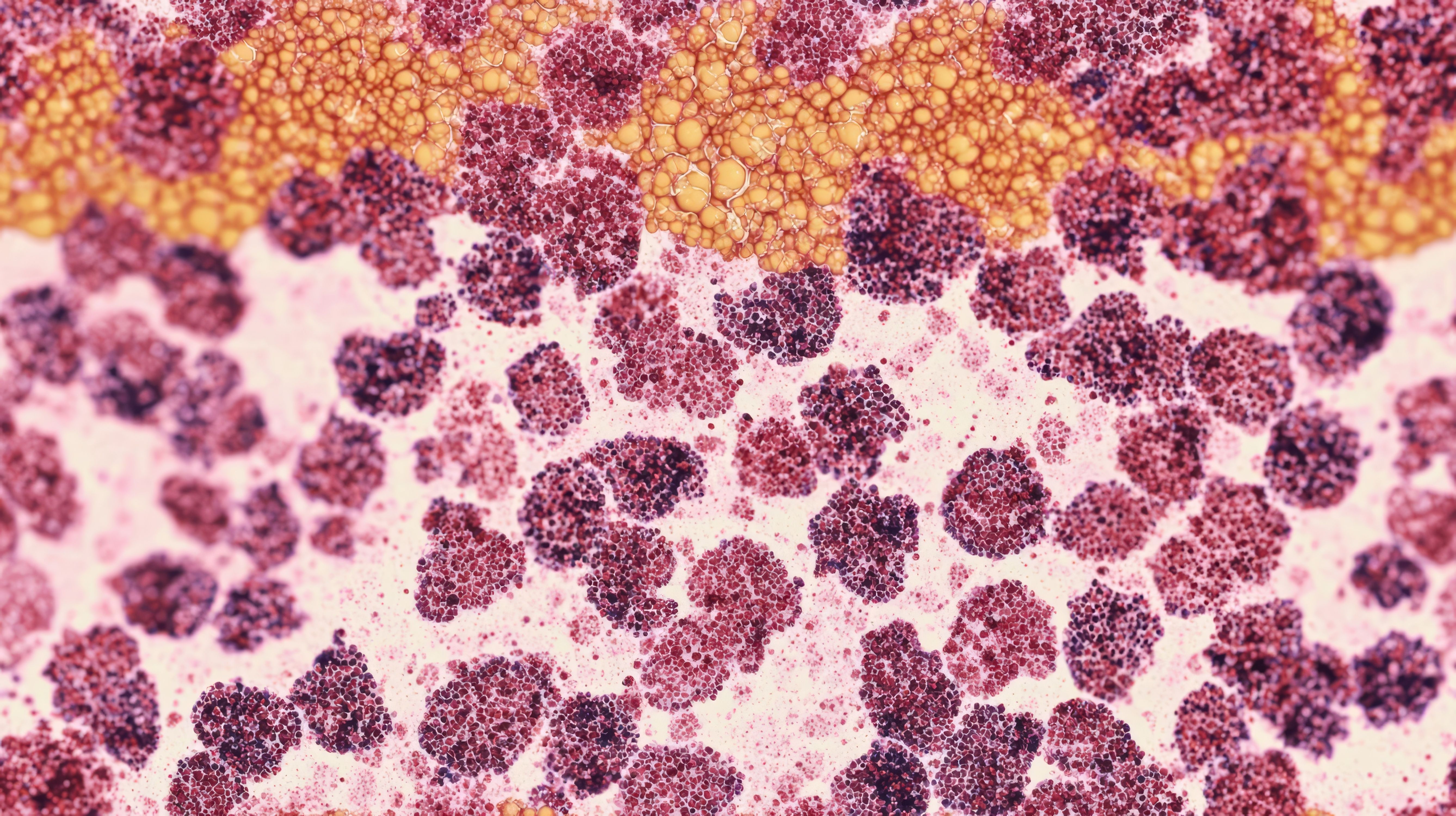
The gut microbiota, separated from the epithelium by a mucus layer, interacts primarily through metabolites that it releases. Image Credit: © Aleksandra - stock.adobe.com

The gut microbiota, separated from the epithelium by a mucus layer, interacts primarily through metabolites that it releases. These metabolites enter systemic circulation and reach different sites in the body, influencing various processes. For instance, certain metabolites can promote inflammation or modulate immune responses, which can subsequently impact cancer development and progression. Healthy gut microbiota balance is essential, as dysbiosis is associated with several cancers, suggesting a link between gut health and tumorigenesis.
“The microbiota, by releasing these metabolites, interacts with the host, and these metabolites can travel across the body in a systemic circulation and can reach different sites. So, most of the activities that we have from the microbiota are dependent on their metabolites,” Rescigno explained during the ESMO session. “But then we have also the intratumoral microbiota, and the intratumoral microbiota has been shown to have an important role both in the development of the tumor… and the activity of the immune response.”
Intratumoral Microbiota
The tumor microbiota is also important for the development of metastases at distant sites and in response to drugs, according to Rescigno. In most cases, the intratumoral microbiota has been associated with negative responses, but can also effect response to therapy.
“The intratumoral microbiota is not only present in colorectal cancer due to the vicinity of the microbiota to the tumor… but also, tumors that are quite far away from the gut have been associated with the intratumoral microbiota,” Rescigno said. “You can see that breast, bone, pancreatic, glioblastoma, ovarian, and lung cancer, as well as melanoma, are full of microbes, suggesting that the microbiota lives within the tumor, and we know that it's also different from adjacent tissue.”
In this way, the microbiota can affect the tumor, but can also affect the immune system, and this has been confirmed in data published by investigators who have analyzed whole genome sequencing, metagenomics, and RNA sequencing, according to Rescigno. Analyzing these data together, investigators observed the microbiota of multiple tumors across various sites and found that microbiota are present in practically every tumor that was analyzed, including mesotheloma, head and neck, liver and bile duct tumors, as well as others.
“We also studied the intratumoral microbiota in the context of sarcoma,” Rescigno said. “Sarcoma has many different histotypes—up to 80 histotypes—and we found that in all of the major sarcoma types, we could find microbiota.”
However, when assessing the presence of microbes in sarcoma through a fluorescence in situ hybridization analysis, Rescigno found that in sarcoma, there are very few microbes within the tumor environment. According to Rescigno, this suggests that there are tumors such as breast cancer that have a significant number of microbes present, while there are others, such as sarcoma, with very few microbes.
“When assessing the microbiota by analyzing 16S rRNA sequencing in the presence of the microbes, you can see that there is an enrichment of microbes within the tumor as compared to the adjacent healthy tissue. This is very important because, since this has a very low biomass, you can have a lot of unspecific analysis of DNA, so you have to make sure that you are really analyzing something that is real,” Rescigno said. “The diversity of this microbiota is different if you compare the healthy tissue from the tumor, and there are also differences according to the histotype in sarcoma.”
Rescigno explained further that when looking at leiomyosarcoma, which is a malignant tumor found in smooth muscle, the diversity of the microbiota of this sarcoma type is not dependent on the location of the sarcoma.
“If you look at the limbs or the trunk [of this sarcoma type], you can see that there are no differences, so it's rather a difference related to the subtype rather than to the location of the tumor,” Rescigno said. “But one important thing considering the tumor antigens is that the microbiota can also be present on the cell surface. So microbial antigens can be present on [major histocompatibility complex (MHC)] class 1 molecules, so this can become a target for T cells.”
Microbial Antigen Presentation
Since microbial antigens from the intratumoral microbiota can be present on tumor cell surfaces via MHC molecules, Rescigno explained that this means that the microbiota can also be used for attacking tumor cells. Notably, this potential is not because they are tumor antigens, but because these are bacterial antigens associated with the tumor. However, this strategy could only be used on a high load microbiota, according to Rescigno. In the case of sarcoma, which has very few bacteria within the tumors, this strategy will likely not work.
Microbiota Tumor Antigen Mimicry
Another possible strategy to use the microbiota in attacking the tumor is through microbiota tumor antigen mimicry, according to Rescigno. It has been shown that there are some microbial antigens that have very high similarity, and sometimes also identity, with tumor antigens. For instance, T cells that recognize microbial antigens might also recognize similar tumor antigens, thereby helping in targeting and killing tumor cells.
“If the immune system is responding to the microbiota, it might also respond to tumors because of the presence of antigen mimicry,” Rescigno said. “Some microbes can [also] induce the release of tumor antigenic peptides. This increases the amount of antigens that can be used for attacking tumors, and also [can be used] for developing vaccines.”
Additionally, research has shown that antibiotics that alter the microbiota can diminish responses to immunotherapy in some cases. Conversely, the introduction of specific beneficial bacteria can restore or enhance the efficacy of treatments such as PD-1 inhibitors, underscoring the intricate relationship between the microbiota and immune system in cancer treatment.
Microbes and ER Stress Response
Some microbes can induce the release of tumor antigenic peptides by exacerbating endoplasmic reticulum (ER) stress in tumor cells, according to Rescigno. Tumor cells, due to their mutations, often have many unfolded proteins, leading to ER stress. When microbes such as Salmonella typhimurium exacerbate this stress, they can increase the presentation of antigenic peptides on the tumor cell surface, thereby enhancing immune recognition and promoting targeted immune responses.
Therapeutic Strategies Involving Microbiota
Overall, there are 3 strategies through which the microbiota can be used to target tumor cells. The first strategy is to target the intratumor on microbiota. With this strategy, it is possible to kill tumor cells because of the presence of tumor antigenic peptides. The advantages of this strategy are that it is possible to avoid tolerance to treatment because these are new antigens that are introduced. However, there are also cons of this strategy, such as in cases where there are very few bacteria in tumor cells, in which case this strategy would need to be personalized to effectively target the tumor cells.
“[For this strategy], you have to know exactly which are the peptides that are presented in the intratumoral microbiota,” Rescigno said.
The second strategy for targeting tumor cells through microbiota is tumor-associated antigen mimicry. In this case, it is necessary to identify peptides that are different from bacteria.
“You have quite a high variety of these peptides, so you have many antigens,” Rescigno said. “This could become universal, so it's not personalized. The only problem you might have is that not all of these antigens might activate an immune response, because you can also have tolerance to the microbiota and [human leukocyte antigen (HLA)] dependency, because you need to activate to bind particular HLA molecules.”
The third strategy uses the release of tumor antigenic peptides. In this strategy, tumor antigens (not coming from the microbiota) the activation of this immune response will attack only ER stress cells and will spare tumor-infiltrating lymphocyte cells.
“This can be universal, because these peptides can be shared by several tumors from the same neoplasm,” Rescigno said. “The only problem here is that they are not easy to be identified, but once you identify them, you can make a universal vaccine.”
Conclusion
The microbiota's involvement in cancer biology offers exciting prospects for developing novel therapeutic strategies. By understanding and manipulating these microbial communities, it becomes possible to enhance the efficacy of existing cancer treatments, reduce adverse effects, and improve patient outcomes. The integration of microbiota analysis into cancer diagnosis and treatment planning may represent a new frontier in precision oncology.
REFERENCE
Rescigno M. Exploiting the microbiome to improve treatment outcomes. ESMO Congress 2024; Barcelona, Spain; September 13-17, 2024.
Newsletter
Stay informed on drug updates, treatment guidelines, and pharmacy practice trends—subscribe to Pharmacy Times for weekly clinical insights.