News
Article
Protecting Pharmacy Technicians: Key Practices in Hazardous Drug Compounding
Author(s):
Key Takeaways
- Hazardous drugs include chemotherapies, antivirals, and hormonal therapies, posing significant reproductive-related adverse effects for patients and health care workers.
- USP <800> outlines guidelines for safe handling of hazardous drugs, emphasizing engineering controls, PPE, and compliance with USP <797> and <795> standards.
Liz Vogel, CPhT-Adv, CSPT, discusses the procedures and best practices for safe compounding of hazardous and non-hazardous drugs.
Drug compounding safety is essential for protecting both patient health and the well-being of pharmacy technicians and other health care workers who handle hazardous medications. At the NCODA Fall Summit in Orlando, Florida, Liz Vogel, CPhT-Adv, CSPT, pharmacy technician instructor from Mayo Clinic, shared crucial information about safety in hazardous drug compounding for pharmacy technicians, covering content including the US Pharmacopeia (USP) <800> standards, the 3 engineering controls, environmental cleaning, and monitoring procedures, as well as the difference in hazardous and non-hazardous drug compounding practices.
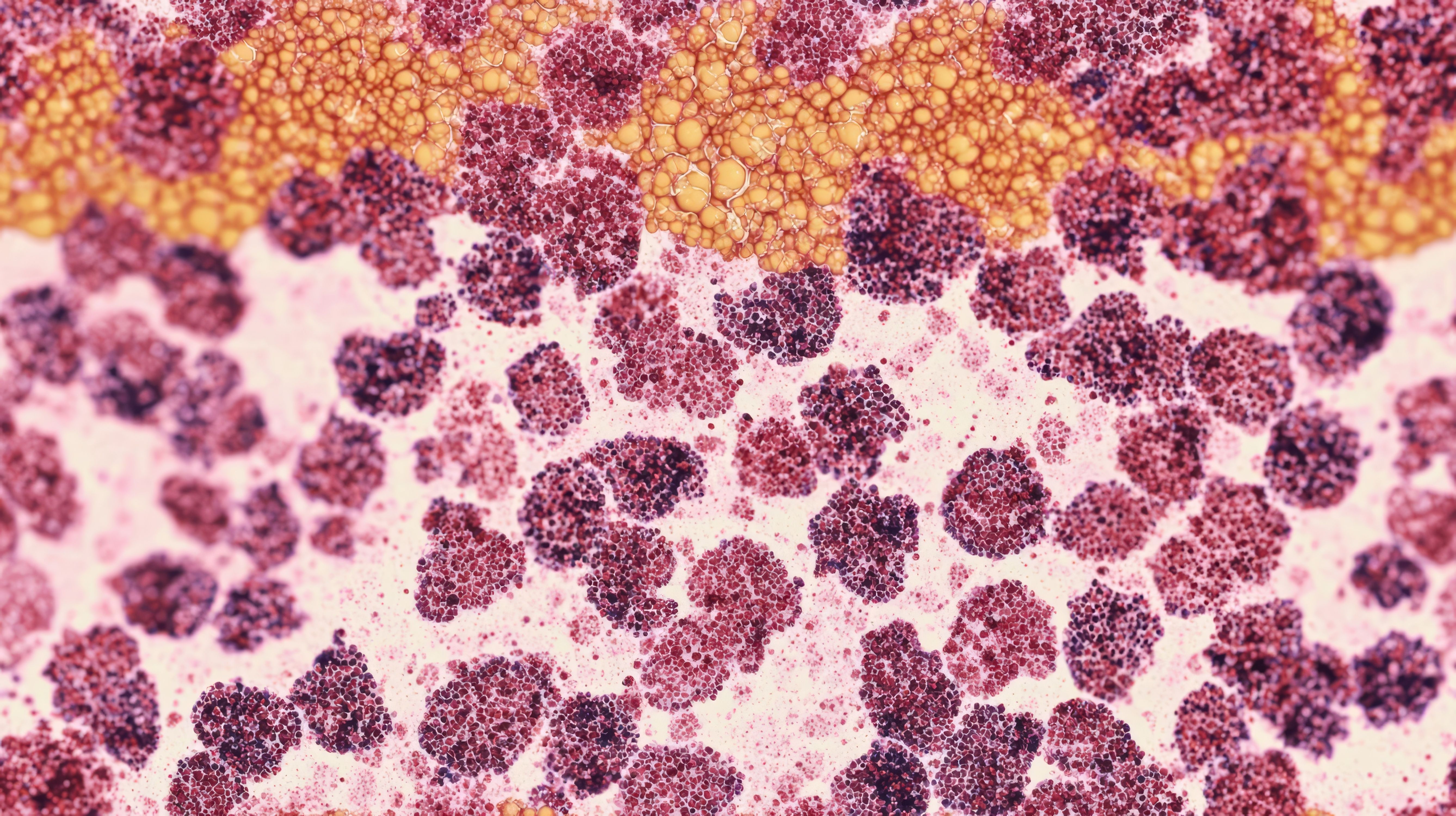
There are differences between hazardous and non-hazardous compounding areas including pressure and air flow, required personal protective equipment (PPE), and cleaning procedures. Image Credit: © JINGWEN - stock.adobe.com

Hazardous drugs are considered any chemotherapies, antivirals, hormonal therapies, or bioengineered products that are capable of binding or damaging DNA, interfere with cell growth or DNA synthesis, and disrupt the function of both healthy and disease cells. All of these result in toxic adverse effects (AEs) for treated patients and their offspring, as well as health care workers. Health care workers may experience skin problems, rashes, allergic reactions, mild hair loss, nail injuries, nasal sores or ocular damage through inhalation, dermal absorption, ingestion, or accidental injection. According to Vogel, the primary characteristic of concern are reproductive-related AEs.
“The first hospital I worked at the [technicians] were terrified to handle any sort of hazardous medication. So, there's definitely a stigma when it comes to that. But we're trying to break the stigma here [through education on and implementation of safe handling protocols] because patients do need these hazardous medications,” said Vogel.
Hazardous drugs are put into 3 categories by the National Institute for Occupational Safety and Health: antineoplastic including cisplatin (Platinol; Bristol-Myers Squibb), cyclophosphamide (Cytoxan; Amneal Pharmaceuticals Inc), and fluorouracil (Tolak; Hill Dermaceuticals); non-antineoplastic such as estrogen, progesterone, or tacrolimus (Prograf; Astellas Pharma Philippines Inc); and drugs with reproductive risks including oxytocin, testosterone, or agents such as warfarin (Jantoven; United Research Labs).
The USP <800> is a section focused on hazardous drug handling in health care settings that applies to pharmacists, nurses, and other personnel, which offer guidance around safe handling, transporting, administering, and disposing of hazardous drugs to ensure patient and technician safety. In addition, USP requires compliance with USP <797> and <795> regarding worker safety in non-sterile compounding of hazardous drugs. These standards state that compounding must be done using proper engineering controls, dedicated disposal, and cleaning equipment for compounding of hazardous drugs and any active pharmaceutical ingredients.
There are differences between hazardous and non-hazardous compounding areas including pressure and air flow, required personal protective equipment (PPE), and cleaning procedures. Hazardous compounding spaces use negative pressure ISO-7 buffer rooms and containment primary engineering controls (C-PEC), as well as require additional PPE. Closed system transfer devices are used to further contain hazardous drugs and environmental monitoring, including surface and air sampling, which are performed more frequently to detect hazardous drug residue.
Compounding of hazardous drugs must be done in a C-PEC to protect against occupational exposure, especially during particle generating activities. This can include the making of intravenous formulations or crushing of tablets resulting in the generation of hazardous particles. Cleaning and decontamination procedures are more stringent, involving deactivation, decontamination, cleaning, and disinfection with sporicidal agents. Vogel suggests following the pyramid, outlining how to limit hazardous drug complications.
“First, you want to try to eliminate it,” said Vogel. “It kind of goes down the pyramid and starts at the top. You eliminate, [but] if you can't do that, you're going to want to substitute. And then if you can't do that, you move down to the 3 that we're going to be talking about today, which are engineering controls, administration administrative controls, or things like standard operating procedures. And then lastly is your PPE. So that's your last line of defense.”
In non-hazardous compounding areas, compounding occurs in a laminar air flow workbench, which provides unidirectional air flow to protect the product, but not the compounder. Unlike hazardous compounding areas, non-hazardous spaces utilize needles and syringes without the need for closed system drug-transfer devices. Environmental monitoring is less frequent, typically limited to monthly microbial surfaces and air sampling, as well as sporicidal cleaning, without the need for daily deactivation and decontamination.
There are 3 engineering controls in drug compounding environments, which include primary, secondary, and supplemental, which are required to protect compounded sterile preparations from cross contamination and microbial contamination. In her discussion of primary engineering controls, Vogel shares her own practice’s layout for drug compounding that consists of an ISO-7 anteroom with an ISO-7 buffer room used for hazardous compounding on one side and an ISO-7 buffer room used for non-hazardous compounding on the other. This layout allows for optimized cleanliness, reduced cross contamination of hazardous and non-hazardous drugs, and reduced exposure for technicians.
Primary engineering controls include biosafety cabinets (BSCs) and compounding aseptic containment isolators that help provide a clean air environment (ie, an ISO-5 or better air quality). BSCs are ventilated to the outside to minimize worker and environmental hazardous drug exposure when directly handling both sterile and nonsterile hazardous drugs. Compounding aseptic containment isolators have unidirectional air flow with a glass shield that trap any generated particles. Primary engineering controls are considered the cleanest compared with secondary and supplemental controls.
“It's important to note that disposable or cleaning equipment for compounding, like your mortars and pestles for nonsterile compounds, must be dedicated for use in this area, and they have to be cleaned appropriately between compounding hazardous and non-hazardous drugs,” said Vogel.
The secondary engineering control is the buffer room where the primary engineering control is located and is physically separate from other preparation areas. The buffer room has fixed walls and is attached to an ISO class 7 anteroom, which provides inward air migration to contain any airborne hazardous drugs with at least 30 air changes per hour. It maintains a negative pressure between 0.01 and 0.03 inches of water column.
Supplemental engineering controls are additional measures used to further contain hazardous drugs, of which the most common example are closed-system drug transfer devices (CSTDs). CSTDs mechanically transfer hazardous drugs and prohibit the transfer of environmental contaminants or escape of hazardous vapors using either a physical barrier or air cleaning technology to prevent exposure. They should be used when compounding hazardous drugs, but they do not substitute for the use of a primary engineering control.
Upon design of a buffer room, it needs to go through a certification process, which can be performed through the Controlled Environment Testing Association or the technician team. Environmental testing and certification approval must be done prior to compounding any category 1 or 2 medications using the controlled environment. The certification covers all classified areas, including the primary engineering control and must be performed every 6 months. Any results that fall out of range should be resolved and then retested.
Environmental monitoring focuses on airflow, high efficiency particulate air filter integrity, and pressure differentials, which are crucial in both hazardous and non-hazardous compounding areas to encourage environmental safety in all compounding areas. It also includes microbial air and surface sampling to identify any potential sources of contamination.
“It's going to tell you how clean or how dirty the area is that you're compounding in, and hopefully, it is cleaner than it is dirty. It is performed using agar plates and then incubated for a set period of time, most of the time for circular sampling,” said Vogel. “It's going to be the 48 hours in an incubator at a higher temperature, and then, it's going to be taken out for 5 to 7 remaining days at a lower temperature. Some sites do their own service sampling and air sampling, and I believe some sites tend to contract that out.”
Regarding cleaning and decontamination procedures, all areas where hazardous drugs are handled must be deactivated, decontaminated, cleaned, and disinfected with sterile isopropyl alcohol or sporicidal agents, according to USP <797>. Technicians, nurses, and other workers should wear appropriate PPE including hair and/or beard covers, face masks, 2 sets of shoe covers, a front closing gown and a back closing laminated gown, eye protection, and 2 sets of sterile powder-free gloves.
In hazardous compounding areas, cleaning is performed from cleanest to dirtiest areas, starting with the primary engineering control. High-touch areas like counters, pass-throughs, and equipment are cleaned and disinfected monthly using sporicidal agents for all surfaces. The floors should also be cleaned with a germicidal product, starting in the furthest corner and mopping towards the exit.
In non-hazardous compounding areas, cleaning is focused on maintaining cleanliness and sterility, without the need for deactivation and decontamination. It typically involves cleaning the laminar air flow workbench using a germicidal agent, disinfecting high-touch areas like counters and equipment, and mopping the floors with a germicidal product. Monthly cleaning using sporicidal agents may be performed but is not as strict as in the hazardous compounding area.
Ensuring the safety of hazardous drug compounding is a collective responsibility that involves adherence to stringent guidelines, specialized equipment, and meticulous environmental monitoring and cleaning practices. By implementing these rigorous procedures, pharmacy teams not only reduce the risk of occupational exposure but also contribute to a safer health care environment for patients and workers alike. A commitment to safety in compounding practices empowers technicians to manage hazardous drugs confidently, fostering a workplace where necessary treatments can be prepared with the highest level of care and protection.
REFERENCE
Vogel, L. Environment matters: ensuring safety in hazardous drug compounding areas. NCODA Fall Summit. October 24, 2024. Orlando, Florida.
Newsletter
Stay informed on drug updates, treatment guidelines, and pharmacy practice trends—subscribe to Pharmacy Times for weekly clinical insights.