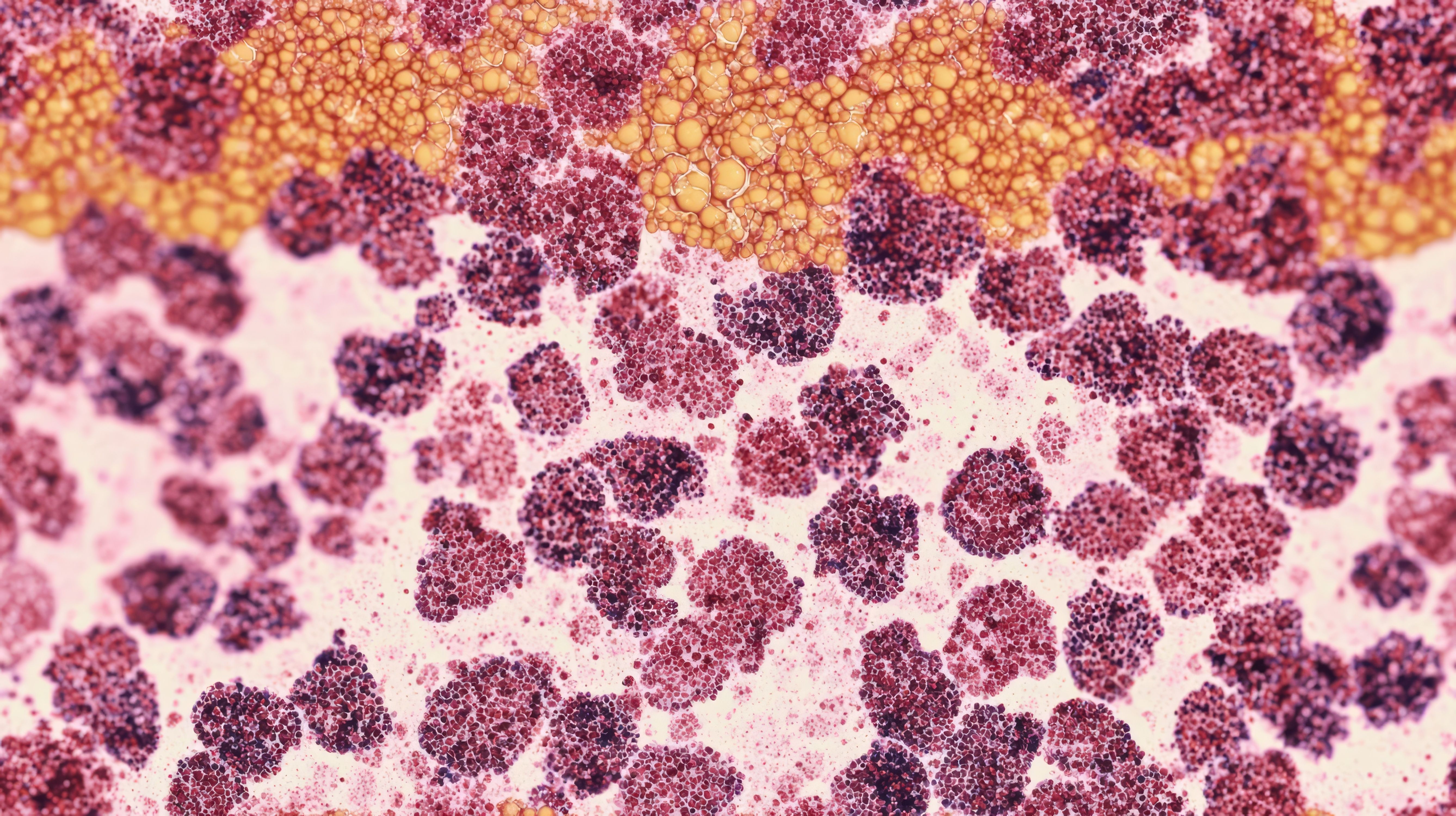
The treatment of relapsed or refractory (R/R) classical Hodgkin lymphoma (cHL) in children and young adults (CAYA) and older adults is constantly fluctuating. While there is variation between the general treatment approach of CAYA and older adults, the overall treatment modality includes biopsy and screening to determine disease severity and whether a complete response (CR) has been achieved, followed by a mix of high-dose therapy and an autologous stem cell transplant (ASCT) with or without radiation therapy, followed by maintenance chemotherapy. Systemic regimens include immune checkpoint inhibitors such as pembrolizumab (Keytruda; Merck & Co) or nivolumab (Opdivo; Bristol Myers Squibb), bendamustine, everolimus, lenalidomide (Revlimid; Bristol Myers Squibb), vinblastine, or brentuximab vedotin (BV; Adcetris; Seagen), a CD30 antibody-drug conjugate. This article highlights the clinical data of BV in combination with nivolumab, bendamustine, or gemcitabine (Gemzar; Eli Lilly) in CAYA and older adult patients with R/R cHL.1,2
BV and Nivolumab in Adult Patients
A phase 1/2 trial (NCT02572167) was conducted evaluating the efficacy of BV and nivolumab as first salvage therapy in 91 adults with R/R cHL. Upon trial initiation, diagnosis staging of the patients was 57%, 18%, and 22% for stages II, III, and IV, respectively. The median age was 34 years, and 92% of patients completed all 4 cycles. At baseline, 13% of patients were determined to have bulky disease and 26% had extranodal disease. On average, patients underwent 1 prior therapy (range, 1-3), including radiation therapy; 30% of patients had relapsed disease within 1 year of frontline therapy completion and 42% had primary refractory disease.3
Following initial staging with PET and CT scans, patients were given up to 4 cycles of BV (1.8 mg/kg) every 3 weeks followed by nivolumab (3.0 mg/kg) in each part of the study. In parts 1 and 2 of the study, patients received the same dosing regimens throughout the cycles. Cycle 1 utilized staggered dosing: BV was given on day 1 and nivolumab was given on day 8. Cycles 2 to 4 utilized same-day dosing: BV and nivolumab were given together on day 1. In part 3 of the study, BV and nivolumab were given on the same day for all cycles. In accordance with the investigator’s discretion, certain patients underwent ASCT immediately after the completion of treatment. Patients who demonstrated progressive disease (PD) were ineligible to continue treatment.3
The primary end point of the study was to assess the safety of the regimen and the antitumor effects demonstrated by the combination of BV and nivolumab. In the absence of prior PD, 18% of patients experienced PD or death. Two patients who achieved CR after therapy did not continue to ASCT due to the onset of Guillain-Barre syndrome. Long-term follow-up of the BV and nivolumab combination has been shown to improve efficacy without additional toxicity.3
After frontline treatment, 3-year progression-free survival (PFS) was 90% (95% CI, 74-96) in the 53 patients with relapsed cHL and 61% (95% CI, 40-76) in the 38 patients with primary refractory disease. CR was achieved in 61 patients; 30 patients did not achieve CR, of whom 16 achieved a partial response (PR). The 3-year PFS of the CR, non-CR, and PR patients was 90% (95% CI, 78-96), 42% (95% CI, 19-64), and 67% (95% CI, 28-88), respectively. Response to treatment was consistent among patients with high and low CD30 tumor expression.3
The ORR was 85%, the CR rate was 67%, and the 3-year overall survival (OS) rate was 93% (95% CI, 85- 97). The highest 3-year PFS rates were demonstrated in the 67 patients who received ASCT therapy directly after 4 cycles of BV and nivolumab. At the median follow-up of 34.3 months, these per-protocol ASCT patients showed improved 3-year PFS rates of 91% (95% CI, 79-96) compared with an estimated 77% (95% CI, 65-86) in the overall patient population. There were 7 deaths, all occurring after the safety reporting period.3
BV and Nivolumab in Pediatric Patients
The multicenter, open-label, phase 2 CHECKMATE-744 study (NCT02927769) assessed the safety and efficacy of BV plus nivolumab in 44 CAYA patients aged 5 to 30 years. Of enrolled patients, 55% were considered to have primary refractory disease after first-line therapy, and 45% had relapsed disease. Notably, the initial diagnosis staging of the patients was 48%, 16%, and 36% for stages II, III, and IV, respectively. All patients received prior systemic therapy and 36% received prior radiation therapy. No patients had a history of BV therapy or ASCT. The median age was 16 years (range, 9-30 years); 70% were 18 years or younger. Criteria for the standard-risk cohort included having 1 or more of the following: primary refractory disease, advanced-stage disease at initial diagnosis, short time to relapse, presence of B-cell symptoms or extranodal disease at relapse, extensive disease, or relapse after radiation therapy.4
Patients received four 3-week cycles of induction treatment with BV and nivolumab: BV (1.8 mg/kg) on day 1 of every cycle and nivolumab (3 mg/kg) on day 8 of cycle 1, then on day 1 of cycles 2 to 4. Patients who did not achieve a CR after 4 cycles of induction received up to four 3-week cycles of intensification with BV and bendamustine (BVB): BV (1.8 mg/kg) on day 1 plus bendamustine (90 mg/m2) on days 1 and 2. Following induction or intensification treatment, patients proceeded to consolidation with high-dose chemotherapy and ASCT if they achieved CR per blinded independent central review (BICR).4
At a minimum follow-up of 15.6 months, the primary end point of CR rate per BICR was 59% after 4 cycles of induction with BV plus nivolumab, 82% after 2 cycles of intensification with BVB, and 94% at any time before proceeding to consolidation. The secondary end point of ORR per BICR any time before consolidation was 100%, with median PFS and OS not reached at time of data cutoff. One patient died due to disease progression.4
BV and Gemcitabine in Pediatric Patients
The Children’s Oncology Group AHOD1221 trial was a single-arm, phase 1/2 study of 46 CAYA patients (aged ≤ 30 years) with primary refractory cHL, high-risk relapsed (relapse ≤ 6 months) or advanced disease (stage III or IV) who were given BV and gemcitabine. The disease stage of the patients prior to BV and gemcitabine initiation was 42% (stages IA, IIA, IIIA), 20% (stages IIB, IIIB), and 38% (stages IVA and IVB).5
In phase 1, the study was designed using the 3+3 dose escalation design with 2 BV doses: 1.4 mg/kg and a second, maximum dose of 1.8 mg/kg. In phase 2, patients received the maximum BV dose that resulted in dose limiting toxicity in less than 33% of patients on day 1 of every 21-day cycle and gemcitabine 1000 mg/m2 on days 1 and 8 of each cycle. Filgrastim (Neupogen; Amgen) was administered to patients with prolonged grade 4 neutropenia or in preparation for peripheral blood stem cell collection.5
The 42 evaluable patients for response analysis were those treated with at least 4 cycles of the phase 2 BV dose and gemcitabine. The combination salvage therapy produced a CR (defined as a Deauville score of 1-2 for all target lesions on fluorodeoxyglucose-PET scan) in 57% of the evaluable patients by the end of the study (95% CI, 41-72) and an ORR of 74% (95% CI, 58-86). As per criteria defined by AHOD1221 protocol for CR, all target lesions with a Deauville score ≤ 3 on central review were considered CRs, resulting in a modified CR rate of 67% (95% CI, 51-80). A post hoc analysis on all evaluable patients resulted in a 1-year OS rate of 95% (95% CI, 80-99). There were a total of 4 deaths reported at 3 or more months after completion of therapy due to either complications from PD or a subsequent treatment.5
BV and Bendamustine in Adult Patients
BV and BVB were analyzed as combination therapy in a phase 1/2 single-arm study (NCT01657331) in 65 adults with R/R cHL. Eligible patients were adults with CD30-positive disease and prior first-line chemotherapy or ASCT. Diagnosis staging of the patients was not provided.6
A total of 28 patients were enrolled in phase 1 of the study. BV was given at a dose of either 1.2 mg/kg or 1.8 mg/kg over 30 minutes on day 1 of each 21-day cycle. Bendamustine was given at doses of either 70 mg/m2, 80 mg/m2, or 90 mg/m2 on days 1 and 2 of the 21-day cycle. Pegfilgrastim was given to prevent myelosuppression per the investigator’s discretion. In this study, patients received up to 6 cycles of BVB. In phase 2 of this study, 37 adults were given the optimal doses of BV (1.8mg/kg) and bendamustine (90 mg/m2).6
The primary end point of the trial was 2-fold. The first was to determine the highest dose for both agents while optimizing adverse effects and toxicity over 1.5 years. The second was to determine the 3-year ORR.6
Between phase 1 and phase 2 of the study, ORR was 61% vs 78%, CR was achieved by 18% vs 43% of patients, and PR was achieved by 43% vs 35% of patients, respectively. In phase 1 and phase 2, PD was observed in 21% and 8% of patients, respectively. The median duration of response was 4.3 months in phase 1 and 3.95 months in phase 2. Of note, the 1-year and 2-year OS rates for phase 2 were 86% and 82%, respectively.6
BV and Bendamustine in Pediatric Patients
A multicenter, retrospective review analyzed the clinical efficacy and safety of BV in 29 CAYA patients (a median age of 21 years) with R/R cHL. The disease staging at initial diagnosis of the patients was 52%, 24%, and 17% for stages II, III, and IV, respectively. At baseline, approximately 48% of patients had bulky disease, 62% had B-cell symptoms, and 14% had extranodal disease.
Patients received a median of 3 cycles of BVB (1.8 mg/kg of BV on day 1 and bendamustine 90 mg/m2 on days 1 and 2 of each 21-day cycle). The median age of the total patient population was 15 years (range, 7-20). Approximately 72% of patients received BVB as first-line salvage therapy and 28% as second-line therapy or later.
The primary end point of CR in patients receiving BVB as first-line salvage therapy was 67% (95% CI, 43-85). The CR rate in patients receiving BVB as second-line therapy or later was 62% (95% CI, 24-91). CR rates were similar among patients with relapsed vs refractory disease (71% vs 58%). The secondary end point of ORR in patients receiving BVB as first-line salvage therapy and second-line or later therapy was 81% (95% CI, 58-95) and 75% (95% CI, 35-97), respectively. Similar to the CR, ORR in patients with relapsed vs refractory disease was 82% and 75%, respectively. The post-BVB event-free survival was 65% (95% CI, 46-85) and OS was 89% (95% CI, 74-100).7
Conclusion
The clinical treatment landscape for adult and CAYA patients is evolving. Incorporating BV therapy with nivolumab, gemcitabine, and bendamustine provides these patients with treatment options that demonstrate promising response rates, improved survival outcomes, and manageable toxicity profiles.
References
About the Authors
Valassia Antigone Theocharides is a 2025 PharmD candidate at the Ernest Mario School of Pharmacy at Rutgers University in Piscataway, New Jersey.
Luisa Giannangelo, RPH, MBA, is a pharmacist and medical writer in High Point, North Carolina.
Jessie Modlin, PharmD, BCOP, is a clinical oncology pharmacist at St Luke’s Cancer Institute in Boise, Idaho.
Tesnim Shash is a 2024 PharmD candidate at the University of Tennessee Health Science Center in Memphis.
Sukeina Nasser, PharmD, RPH, CPH, PACS, is a clinical pharmacist in Detroit, Michigan.
1. NCCN. Clinical Practice Guidelines in Oncology. Hodgkin lymphoma, version 2. 2023. Accessed January 16, 2024. https://www.nccn.org/guidelines/guidelinesdetail?category=1&id=1439
2. NCCN. Clinical Practice Guidelines in Oncology. Pediatric Hodgkin lymphoma, version 2. 2023. Accessed January 16, 2024. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1498
3. Advani RH, Moskowitz AJ, Bartlett NL, et al. Brentuximab vedotin in combination with nivolumab in relapsed or refractory Hodgkin lymphoma: 3-year study results. Blood. 2021;138(6):427-438. doi:10.1182/blood.2020009178
4. Harker-Murray P, Mauz-Körholz C, Leblanc T, et al. Nivolumab and brentuximab vedotin with or without bendamustine for R/R Hodgkin lymphoma in children, adolescents, and young adults. Blood. 2023;141(17):2075-2084. doi:10.1182/blood.2022017118
5. Cole PD, McCarten KM, Pei Q, et al. Brentuximab vedotin with gemcitabine for paediatric and young adult patients with relapsed or refractory Hodgkin’s lymphoma (AHOD1221): a Children’s Oncology Group, multicentre single-arm, phase 1-2 trial. Lancet Oncol. 2018;19(9):1229-1238. doi:10.1016/S1470-2045(18)30426-1
6. O’Connor OA, Lue JK, Sawas A, et al. Brentuximab vedotin plus bendamustine in relapsed or refractory Hodgkin’s lymphoma: an international, multicentre, single-arm, phase 1-2 trial. Lancet Oncol. 2018;19(2):257-266. doi:10.1016/S1470-2045(17)30912-9
7. Forlenza CJ, Gulati N, Mauguen A, et al. Combination brentuximab vedotin and bendamustine for pediatric patients with relapsed/refractory Hodgkin lymphoma. Blood Adv. 2021;5(24):5519-5524. doi:10.1182/bloodadvances.2021005268