Publication
Article
Pharmacy Practice in Focus: Oncology
Navigating the Complexities of NSCLC Treatment: The Clinical and Economic Impact of Care
Author(s):
The financial burden has increased significantly since 2015.
Treatment for lung cancer today requires a multimodal approach, explained Scott Soefje, PharmD, MBA, BCOP, FCCP, FHOPA, director of pharmacy cancer care at Mayo Clinic in Rochester, Minnesota, during a Pharmacy Times Clinical Forum panel discussion.
Although surgery remains the best chance for cure in stage I or II non–small cell lung cancer (NSCLC), other options can extend life, Soefje explained.
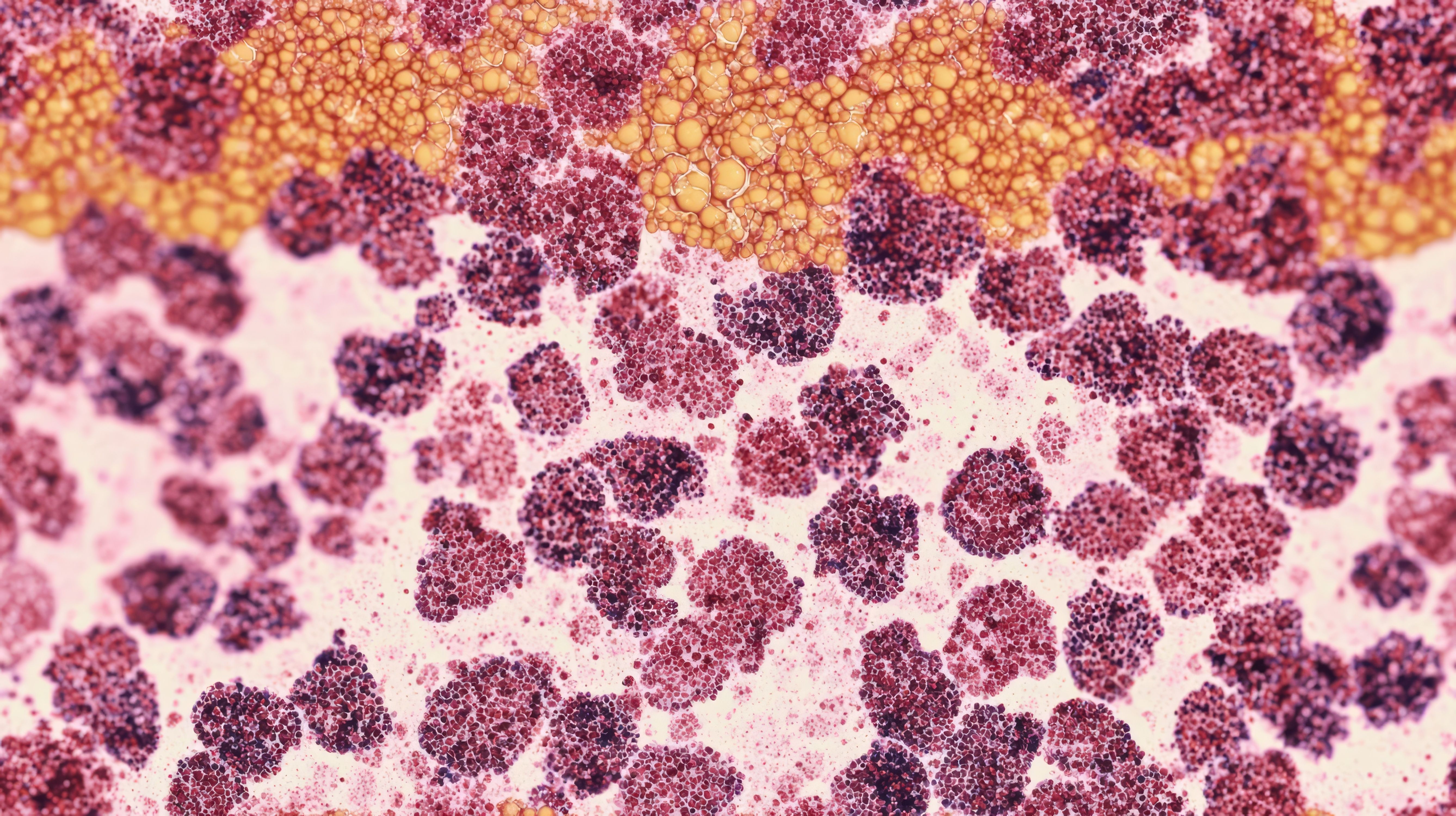
Image credit: methaphum | stock.adobe.com

“As I always tell residents, if we’re going to cure somebody with lung cancer, we’re going to have to cut it out,” Soefje said. “There used to be a time when that was the only chance for cure, but I think we may see some changes in the way things are done [in that regard].”
The choice of surgery for patients with NSCLC is determined by the patient’s ability to tolerate surgery and is dependent on the extent of the disease and cardiopulmonary reserve of the patient. After surgery, radiation is often a second choice for treatment and plays a potential role in all stages of NSCLC treatment, according to Soefje. However, Soefje noted that pharmacists who work with patients with lung cancer may observe interesting interactions among radiation therapy, immunotherapy, and chemotherapy in patients, which requires monitoring.
Definitive radiation can be used for patients with locally advanced NSCLC, according to Soefje. Definitive radiation can also be used if surgery is not available or can be used in the neoadjuvant or adjuvant setting for patients treated with surgery, Soefje explained. Further, definitive radiation can be used to help patients get to surgery or as adjuvant therapy following surgery. Additionally, palliative radiation can be used for patients with incurable NSCLC as well, according to Soefje.
When patients with NSCLC are not eligible for targeted therapy or immunotherapy, platinum-based chemotherapy is recommended. “Platinum-based chemotherapies are still the backbone [of treatment, but] we’re starting to see more of the targeted-type therapies and immunotherapies even in the front line with higher response rates, and we’ve moved into the immunotherapy- and chemotherapy-type realm as we’ve gone forward,” Soefje said. “This is a great area for your precision medicine people.”
Soefje explained that Mayo Clinic made a conscious decision when it started the precision medicine process to put a pharmacogenomics professional into the cancer group. Soefje explained there were some protestations at first with this addition, but these were resolved once the value of a pharmacogenomics perspective on complex patient cases was made clear.
Although immunotherapy and targeted therapies have shown higher response rates and better tolerance for patients than chemotherapy, the cost of treatment is an additional factor that can be impactful for patients.
“Lung cancer is not cheap. If you haven’t looked, there is significant financial toxicity [for patients with NSCLC]. I find it interesting [that] financial toxicity wasn’t even a term until 2011, and now it’s one of the more common ones you’re starting to see,” Soefje said.
However, financial toxicity from lung cancer treatment may not be due to the high cost of drugs alone, Soefje explained. “There are high costs of drugs, but there [are] also a lot of nonmedical costs,” Soefje said. “Has anyone ever at your institution sat down and figured out what it costs to come to your institution just to get chemotherapy or an infusion? We did. And it’s $200 a day—and this counts time away from work and that kind of stuff.”
Soefje explained that this number increases significantly depending on whether the patient needs to travel to Mayo Clinic for treatment, which would add costs related to overnight stays, airfare or gas, and other related travel costs. “It jumps up to $400 to $1000 depending on [whether] you have to spend the night and how far you have to travel. That’s pretty significant,” Soefje said.
Soefje noted the cost of care per day can also depend on the caregivers the patient is bringing, which can add hotel stays or airfare costs. “But we estimate on average for our patients, it’s about $400 for the patient to come in, [and that’s] for the nonmedical costs,” Soefje said.
For the medical costs, the National Cancer Institute (NCI) has reported overall costs will increase 34% or more from 2015 to 2030.1 Specifically, NCI showed that in 2015, the total cost of cancer treatment in the US was $190.2 billion, and in 2020 this number jumped to $208.9 billion.1 In lung cancer, the total cost was $21.2 billion in 2015 and $23.8 billion in 2020.1 By 2030, an estimated minimum increase of 34% from these 2015 figures will be significant, Soefje explained.
For patients, the annual cost of care per patient with lung cancer ranges from $12,200 to $118,000, according to Boulanger et al in a 2022 study published in Frontiers in Oncology.2 According to these authors, the greatest financial burden occurs at the time of initial diagnosis and in the last year of life.2
“I remember when the annual cost of care would hit $1000 a year, and it was notable. Now it’s 10 times that per month at this point in time. If you’ve never looked at the data, the actual cost per drug passed the median household income in the United States in 2005, and it just continues to grow,” Soefje said. “Medical debt is the leading cause of bankruptcy in this country, and it’s a significant problem. So the economic impact is something we’re all going to be faced with.”
When pharmacists are looking to counsel patients on their treatment and care, Soefje noted an optimal time for this can be while the patient is receiving intravenous (IV) therapy. “I liked [counseling patients] in the chair because they are kind of a captive audience,” he said.
Clinical Forum panelist Sophia Gilardone, PharmD, BCOP, oncology pharmacy specialist of the University of Pennsylvania, explained that providing patient education while they are receiving IV infusion is often also beneficial because it usually is not the first time they will be receiving that information, but it can be a time where they might truly retain that information.
“At that point they’ve already been told it once, so this is our time to [help them] digest it rather than talking to them all at one time when their heads are racing anyway,” Gilardone said.
Additionally, Gilardone explained that she will sometimes step in to make a recommendation for treatment that counters that of the physician, although this is generally a rare occurrence.
“We have a great team, and they are typically making really sound decisions. But there are times where I’m like, ‘Hey, especially when there [are] so many oral [treatments], there’s a drug interaction that makes this option better than that one,’” Gilardone said. “I will also get involved too if there may be an impact on renal function, for example.”
Gilardone explained that often a physician may sit down with her to discuss options for treatment, especially after trying several therapies without achieving results. Additionally, she sits on the tumor board, which includes a multidisciplinary team.
The treatment landscape for lung cancer continues to evolve with a multimodal approach that integrates surgery, radiation, chemotherapy, targeted therapies, and immunotherapy. Pharmacists play a vital role in patient education and monitoring, ensuring optimal treatment outcomes and helping patients address the economic impact of care. As precision medicine advances, integrating pharmacogenomics into cancer care may further enhance treatment efficacy and patient quality of life.
REFERENCES
1. National Cancer Institute. Financial burden of cancer care. Cancer Trends Progress Report. National Institutes of Health; updated March 2024. Accessed July 19, 2024. https://progressreport.cancer.gov/after/economic_burden
2. Boulanger M, Mitchell C, Zhong J, Hsu M. Financial toxicity in lung cancer. Front Oncol. 2022;12:1004102. doi:10.3389/fonc.2022.1004102

Newsletter
Stay informed on drug updates, treatment guidelines, and pharmacy practice trends—subscribe to Pharmacy Times for weekly clinical insights.
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.