Lotilaner a Breakthrough Drug in Demodex Blepharitis Treatment
Key Takeaways
- Lotilaner 0.25% is the first and only FDA-approved medication that specifically targets Demodex mites. Its effect depends on twice-daily adherence for 6 weeks.
- Clinical trials have proven the drug’s safety and efficacy, with results showing significant mite eradication, reduction in redness and inflammation, and collarette resolution.
Demodex blepharitis is a common condition of eyelid inflammation. Lotilaner is the first FDA-approved, targeted treatment, offering effective mite eradication with minimal side effects.
Blepharitis is an inflammatory condition of the eyelids that develops due to bacterial etiology or, more commonly, demodex mite infestation.¹ This condition is common, affecting about 25 million Americans, and is more commonly seen in older adults and immunocompromised patients. The presentation of demodex blepharitis is characterized by redness, itchiness, and dryness, with some patients experiencing swelling, loss of eyelashes, discharge, or irritation.
Until July 2023, the strategies for managing chronic eyelid inflammation included the use of over-the-counter (OTC) products, non-specific prescription drugs, and non-pharmacological therapies.
A New Drug, and the First in its Class
Lotilaner (Xdemvy/Tarsus Pharmaceuticals, Inc.) is the first and only FDA-approved drug for the treatment of demodex blepharitis. Lotilaner 0.25% is manufactured as a 10 mL ophthalmic solution, dosed as 1 drop in each eye twice daily for a duration of 6 weeks.² The drug is an antiparasitic agent that acts as a GABA-gated chloride channel inhibitor in the mites, resulting in paralysis and death. It is stored at room temperature, has no contraindications, and no known drug interactions, with adverse effects limited to burning and stinging of the eyes after administration, as well as chalazion or stye formation.
Previous Management Strategies
Prior to lotilaner’s approval, patients were limited to few prescription medications (with limited efficacy) and OTC products to manage blepharitis symptoms. A prescription combination of ivermectin and metronidazole has been used off-label to reduce mite density and improve symptoms.¹ The mechanisms of these drugs, however, are non-specific to mite eradication, which increases the risk of side effects. Ivermectin is an antiparasitic agent that comes in topical and oral forms. The topical form is not safe for administration in the eye. The oral form may have benefits in reducing mite density, but its systemic activity increases the risk of side effects, which include neurotoxicity, CNS depression, and immunologic reactions.
Similar statements can be made for Metronidazole’s topical and oral forms. With a mechanism that targets bacteria and parasites, it may benefit patients with demodex blepharitis; however, its oral systemic administration increases the risk of side effects, including nausea, vaginitis, CNS effects, and GI discomfort.
Tea tree oil is an OTC product often utilized to manage mite infestation in the eyelashes due to its broad-spectrum antimicrobial activity.¹ Some formulations have shown modest levels of mite eradication and improvement in symptoms of inflammation; they come in 3%-100% concentrations as a gel, shampoo, ointment, scrub, or other form. It is worth noting that side effects are seen in the use of higher concentrations of tea tree oil, including contact dermatitis, ocular irritation, and allergic reactions.
Lastly, products such as eyelid scrubs, lubricating eye drops, eye itch relief eye drops, or lubricating ointments have also been utilized for symptom management. Though these agents do not address the source of the problem, they do provide patients with temporary relief.
Trials that Led to FDA Approval
Two phase 3 randomized clinical trials (SATURN-1 and SATURN-2) provided the data that led to FDA approval.³,⁴ In the SATURN-1 trial, patients with demodex blepharitis were assigned to receive lotilaner or a placebo twice daily for 43 days.3 The results showed statistically significant improvement in collarette cure (81.3% vs. 23.0%), mite eradication (67.9% vs. 17.6%), and erythema cure (19.1% vs. 6.9%) in the treatment group. Adverse effects were mild, mainly administration site irritation. The SATURN-2 trial design was similar to the first study, with a study duration of 6 weeks.4 The results similarly showed statistically significant improvement in collarette cure (56.0% vs. 12.5%), mite eradication (51.8% vs. 14.6%), and erythema cure (31.1% vs. 9.0%).
Access to Lotilaner
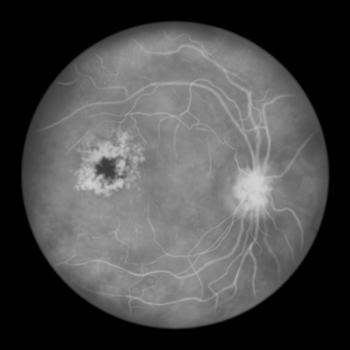
Lotilaner is available via prescription only. Patients should be referred to an ophthalmologist if demodex blepharitis is suspected, where diagnostic testing includes visualizing the collarette, or waxy debris, accumulation at the base of the eyelashes using a slit lamp.5 Currently, lotilaner is only available at select Specialty pharmacies such as Walgreens Specialty Pharmacy, CVS Specialty Pharmacy, and BlinkRx.6 In 2025, the cash price for a 10mL bottle is $ 2,394.² A co-pay card is available on the manufacturer’s website for patients with commercial insurance, which covers up to $2,000 of the copay.
Patient Counseling
- Separating from eye products. Due to its formulation as an eye drop, it is critical to counsel patients on the proper administration technique. Some providers may include directions to rub on eyelashes, but it is not necessary. Instilling eyedrops directly into the eye will allow adequate application to the eyelid margin. Many patients initiating lotilaner have already begun utilizing OTC products to control the symptoms of blepharitis. This is where the pharmacist's role in counseling proves important. The patient should be educated on separating lotilaner from other eye drops for 5 minutes and removing contact lenses before administration, then waiting 15 minutes before reinserting.²
- Dispensing refills. One bottle of lotilaner contains enough solution for 50 days of therapy, whereas the patient only needs 42 days. The manufacturer incorporates overfill within the 10mL bottles, allowing patients with dexterity issues to complete the 6 weeks without gaps in therapy. Patients typically follow up with their eye-care provider for re-evaluation once the course is complete; they may then decide whether a second course is needed. From the trials, Xdemvy is ~50-60% effective in mite eradication.
- Duration and adherence. Patients must adhere to twice-daily administration for the duration of treatment, as missed doses may compromise medication efficacy. The life cycle of demodex mites is 14-23 days, with studies indicating the 6-week period to be the optimal duration to target the eggs, adult mites, and the reproductive process to clear the infestation.¹
- Use of Make-up. The package insert does not discuss the need to avoid eye makeup during the treatment course. Avoiding eye makeup can lessen irritation while inflammation is managed.7 If using makeup, remove it thoroughly before going to bed. Patients may also choose to replace their mascara/ makeup at the end of their treatment course to reduce recurrence.
- Is demodex contagious? Demodex infections are chronic conditions that are not usually contagious.7
- Do I need to change my bedsheets? Counsel on changing bedsheets, pillow cases, and towels weekly to prevent recurrence. Wash them in hot water to kill off the mites.
- How the infestation occurs. A diagnosis of demodex blepharitis is not necessarily related to the patient’s hygiene, but it can be a factor in its development.7 Environmental factors and local changes can cause the reproductive habits of the mites to change and increase. In many instances, patients diagnosed with demodex blepharitis have recalled specific triggering factors that may have caused the infestation. Some situations include a recent move, a recent cruise, or cleaning a dusty attic.
REFERENCES
1. Rhee MK, Yeu E, Barnett M, et al. Demodex Blepharitis: A Comprehensive Review of the Disease, Current Management, and Emerging Therapies. Eye Contact Lens. 2023;49(8):311-318. doi:10.1097/ICL.0000000000001003
2. Xdemvy. In: Lexi-Drugs. UpToDate, Inc.; 2025. Updated September 5, 2025. Accessed September 9, 2025. http://online.lexi.com
3. Yeu E, Wirta DL, Karpecki P, Baba SN, Holdbrook M; Saturn I Study Group. Lotilaner Ophthalmic Solution, 0.25%, for the Treatment of Demodex Blepharitis: Results of a Prospective, Randomized, Vehicle-Controlled, Double-Masked, Pivotal Trial (Saturn-1). Cornea. 2023;42(4):435-443. doi:10.1097/ICO.0000000000003097
4. Gaddie IB, Donnenfeld ED, Karpecki P, et al. Lotilaner Ophthalmic Solution 0.25% for Demodex Blepharitis: Randomized, Vehicle-Controlled, Multicenter, Phase 3 Trial (Saturn-2). Ophthalmology. 2023;130(10):1015-1023. doi:10.1016/j.ophtha.2023.05.030
5. Mukamal R. Are Tiny Mites Causing Your Blepharitis? Am. J. Ophthalmol. Published March 15, 2022. Accessed September 9, 2025. https://www.aao.org/eye-health/tips-prevention/demodex-mites-blepharitis-itchy-red-eyelid-eyelash
6. Tarsus Pharmaceutical, Inc. Savings and Access. Xdemvy. Accessed September 9, 2025. https://xdemvy.com/savings-and-access
7. Blepharitis. Cleveland Clinic. Reviewed December 20, 2022. Accessed September 9, 2025. https://my.clevelandclinic.org/health/diseases/10032-blepharitis
Newsletter
Stay informed on drug updates, treatment guidelines, and pharmacy practice trends—subscribe to Pharmacy Times for weekly clinical insights.