Collaboration Allows Pharmacy Employees to Increase Vaccination Rates
Staff members, especially immunizers, should look at every encounter as an opportunity to educate, support patients.
For many pharmacists, making immunization recommendations is a daily need but a daunting task.
A few tips can make recommendations easier. These include the following:
Know who needs what. Every immunizer needs access to the CDC’s immunization schedules, which are a click away.1 They include the Advisory Committee on Immunization Practices (ACIP) recommendations for immunizations by age. That same link provides patient-friendly schedules. Printing schedules for patients to take home and note on the family’s calendar can emphasize that immunization is a journey, not a destination.1
Know the lingo. Patients need all kinds of immunizations. Aspharmacists look at a patient’s immunization record, they should ask3 screening questions1,2:
- Does this patient need any routine immunizations?
- Has this patient missed routine immunizations and do they need catch-up immunizations?
- Does this patient have risk factors that fall into the risk-based recommendations?
If the answer to any of these questions is yes, the default decision should be to vaccinate according to ACIP recommendations unless the vaccine is contraindicated for a specific patient.1
Use teachable moments. Teachable moments are opportunities to teach using real-world current events.3 When vaccine-preventable outbreaks occur, that is the teachable moment to ask whether patients are fully immunized.
Work with the pharmacy team.4Team members who seem to charm the spots off a leopard may be the best representatives to encourage patients to be vaccinated. Ideal employees are cheerful, empathetic, and trustworthy individuals who like and want the best for patients.
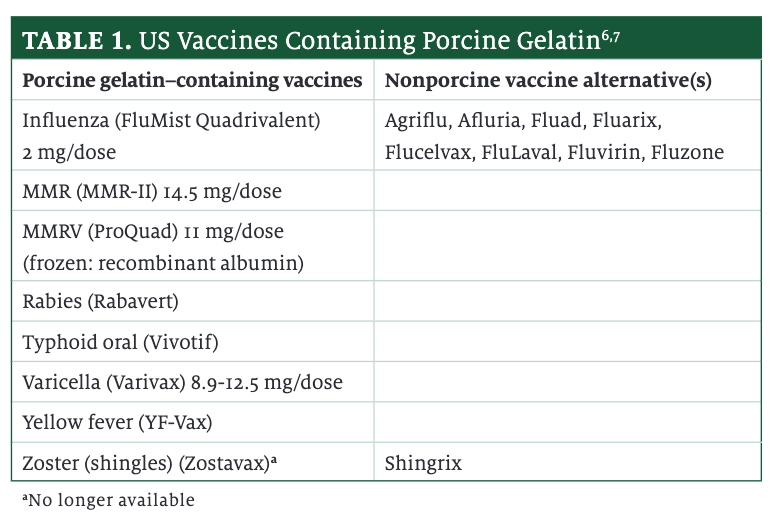
Be confident and strong. Patients are much more likely to be immunized if a health care provider recommends the vaccine and uses strong language.5 The difference between “You should receive these vaccinations” and “I strongly recommend the flu shot and the COVID-19 shot this year. They save lives” is enormous. Some patients will refuse immuni-zations because they perceive they will violate their dietary or religious restrictions. Knowing which vaccines contain or used to contain gelatin or pork and the alternatives(Table 16,7) can alleviate patients’ fears. Reassuring patients that a porcine-containing vaccine is no longer used and a different option is available may be all that is needed to move them from hesitancy to acceptance.
Be persistent. Patients sometimes offer excuses when offered a vaccination. The excuses may be flimsy or scientifically unsound, and persistence often pays off.8
Be clear. When talking to patients about vaccinations, it is best to skip the fancy language and jargon. Use phrases and words that patients will understand. Immunizers should correct misinformation immediately if patients say something that is clearly wrong.9-11 Instead of saying that something is incorrect, immunizers need to fill the patient’s information gap with an alternative, evidence-based explanation. If the situation calls for the immunizer to repeat the misinformation, it is critical to state explicitly that the information is false. It can help to explain why it is wrong and why many believe the misinformation. Finally, keeping explanations short is smart; convoluted or long explanations often push the patient back toward the easier-to-understand misinformation.9-11
Be inclusive. Sometimes, letting patients know they can bring their family and friends with them has an advantage. Many patients find comfort in having others around them.
Remember to share. The ACIP does not recommend all vaccinations for everyone based simply on age or identifiable risk group.2 For these vaccines called shared clinical decision-making vaccinations (Table 22), broad vaccination of individuals in that group is unlikely to have population-level impacts; that is, herd immunity is off the table. Clinicians administer these vaccines after a thoughtful discussion with the patient or a parent or guardian. The ACIP advises clinicians to cover several factors: the best evidence describing the vaccine’s benefits; the immunizer’s clinical discretion; the individual’s characteristics, preferences, and values; and the specific vaccine’s characteristics.2
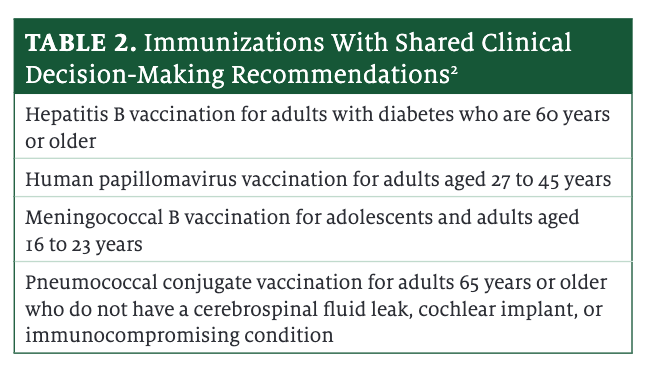
Know who pays. Under the Affordable Care Act, patients will not owe coinsurance or a co-pay or have a deductible if the CDC has adopted ACIP recommendations “with respect to the individual involved” and the CDC lists the vaccine on its immunization schedules. Health plans and insurers cannot impose any cost-sharing requirements even if the ACIP recommends the vaccine with shared clinical decision-making.12
Conclusion
Immunizations can be complicated and laden with emotion for patients. Immunizers should look at every encounter as an opportunity to educate and support patients. Pharmacy staff members can work collaboratively to increase community vaccination rates.
References
1. Immunization schedules. CDC. Updated February 10, 2023. Accessed February 15, 2023. https://www.cdc.gov/vaccines/schedules/index.html
2. ACIP shared clinical decision-making recommendations. CDC. Updated February 10, 2023. Accessed February 15, 2023. https://www.cdc.gov/vac-cines/acip/acip-scdm-faqs.html
3. Wosniak S. Motivating students with teachable moments. Association for Middle Level Education. August 2014. Accessed February 6, 2023. https://www.amle.org/motivating-students-with-teachable-moments/
4. Berg S. How to get patients on board with immunization. American Med-ical Association. September 28, 2018. Accessed February 6, 2023. https://www.ama-assn.org/delivering-care/public-health/how-get-patients-board-immunization
5. Healy CM, Savas LS, Shegog R, Lunstroth R, Vernon SW. Medical ethics principles underscore advocating for human papillomavirus vaccine. Hum Vaccin Immunother. 2022;18(1):1989926. doi:10.1080/21645515.2021.1989926
6. Vaccines licensed for use in the United States. FDA. July 5, 2022. Accessed February 6, 2023. https://www.fda.gov/vaccines-blood-biologics/vaccines/vaccines-licensed-use-united-states
7. Vaccine ingredients - gelatin. Children’s Hospital of Philadelphia. Updated September 6, 2022. Accessed February 15, 2023. https://www.chop.edu/centers-programs/vaccine-education-center/vaccine-ingredients/gelatin
8. Fogarty CT, Crues L. How to talk to reluctant patients about the flu shot. Fam Pract Manag. 2017;24(5):6-8.
9. Lewandowsky S, Ecker UKH, Seifert CM, Schwarz N, Cook J. Misinformation and its correction: continued influence and successful debiasing. Psychol Sci Public Interest. 2012;13(3):106-131. doi:10.1177/1529100612451018
10. Dubé E, Gagnon D, Vivion M. Optimizing communication material to address vaccine hesitancy. Can Commun Dis Rep. 2020;46(2-3):48-52. doi:10.14745/ccdr.v46i23a05
11. Ecker UK, Lewandowsky S, Tang DT. Explicit warnings reduce but do not eliminate the continued influence of misinformation. Mem Cognit. 2010;38(8):1087-1100. doi:10.3758/MC.38.8.1087
12. Section 2713(a)(2) of the Public Health Service Act, as added by section 1001 of the Affordable Care Act, implemented at 26 CFR 54.9815-2713(a)(1)(ii), 29 CFR 2590.715-2713(a)(1)(ii), and 45 CFR 147.130(a)(1)(ii).
About the Author
Jeanette Y. Wick, MBA, RPh, FASCP is the director of pharmacy professional development in the Department of Pharmacy Practice at the University of Connecticut School of Pharmacy in Storrs.