About the Author
Jeannette Y. Wick, MBA, RPh, FASCP, is the director of pharmacy professional development in the Department of Pharmacy Practice at the University of Connecticut School of Pharmacy in Storrs.
Antimicrobial stewardship is crucial for all health care professionals—not just those in a hospital setting
Antimicrobial stewardship programs (ASPs) are alive and well, but so is antimicrobial resistance (AMR). Annually, more than 2 million Americans contract infections resistant to customary treatment, and experts estimate that by 2050, these infections will cause 10 million deaths globally every year. In fact, AMR continues to significantly increase morbidity, mortality, and health care costs despite the growth of ASPs.1,2
Image credit: nobeastsofierce | stock.adobe.com

Misuse of antimicrobial medications is the primary culprit.1,2 Other causes include self-medication with antibiotics, agricultural and livestock antibiotic use, and pollution of water sources with sewage runoff or industry waste.3-5
Jeannette Y. Wick, MBA, RPh, FASCP, is the director of pharmacy professional development in the Department of Pharmacy Practice at the University of Connecticut School of Pharmacy in Storrs.
TAKING THE ASP HELM
ASPs strategize to optimize antimicrobial use, improve patient outcomes, and stop or delay the emergence of resistance.6,7 By definition, ASPs are multidisciplinary in nature, involving infectious disease physicians, infection control professionals, hospital epidemiologists, and pharmacists.7 Pharmacists on ASPs use their expertise to perform indispensable duties, and study findings indicate that pharmacist-led interventions significantly improve prescribing practices, reduce unnecessary antibiotic use, optimize antibiotic selection and therapy, and enhance patient clinical outcomes.7-9
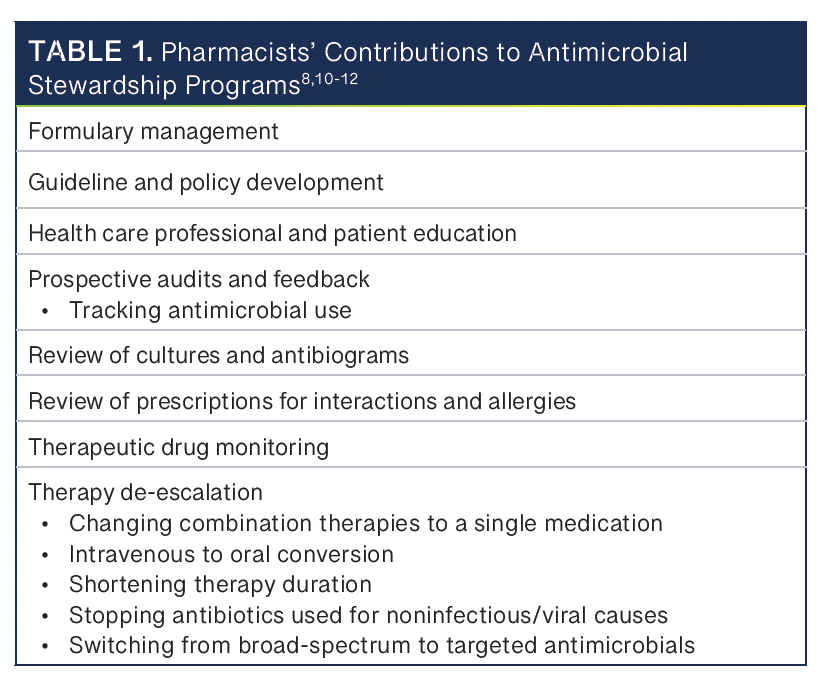
Most ASPs are established in hospital or clinic settings, but there is also a great need for stewardship in the community. Community based pharmacists can conduct some of the activities listed in Table 1.8,10-12 Perhaps the most significant responsibilities in community settings are the education of both health care professionals and patients, prescription review for interactions and allergies, and occasionally recommending therapy de-escalation.
EDUCATING THE RELUCTANT PATIENT OR CAREGIVER
Community pharmacy staff may interact with patients who are unhappy with a prescriber’s refusal to write a prescription for an antimicrobial. Parents who want an antibiotic for a child’s ear infection (a practice that has fallen out of favor) are an example. Often patients need to understand situations on a personal level before they understand the problem’s urgency and embrace solutions. One way to bring home the message that antimicrobial overuse has repercussions is by raising awareness of antibiotic adverse events (AEs), emphasizing consequences of misuse, and explaining irreversible environmental effects.
ADVERSE EVENTS ARE CONCERNING
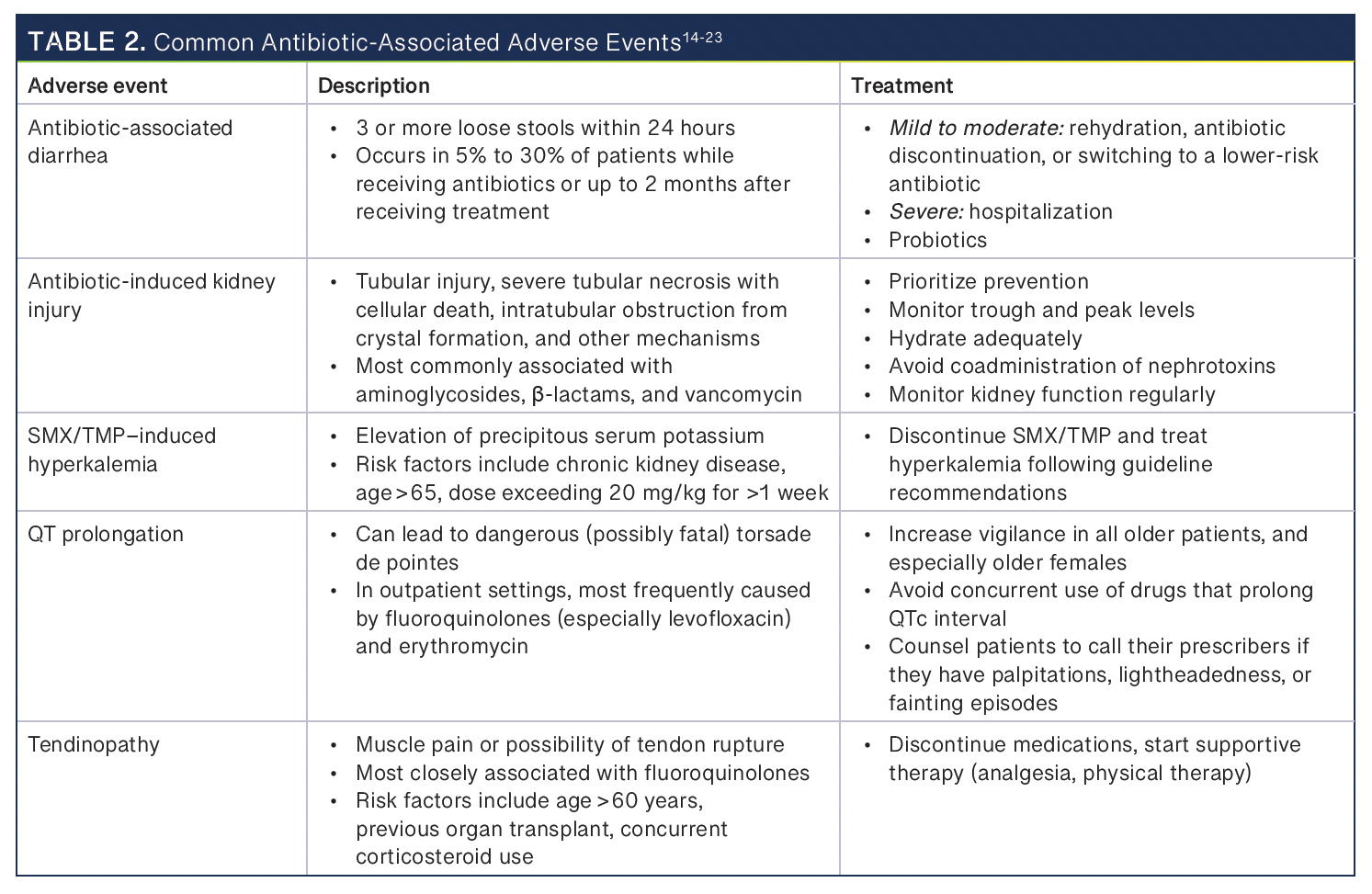
Antibiotics are the drug class most likely to cause AEs. More than 30% of children who take antibiotics for 14 days or more experience an AE.13 Many adults do too. Most antibiotic effects are mild and self-limiting, but diarrhea and rash can be signals that more severe AEs are possible.13 Discussing the possibility—or the likelihood—of AEs can help patients understand personal risks.Table 214-23 shows several AEs.
Another area where community pharmacists can be stewards is in topical treatment.24-26 OTC topical antibiotics such as bacitracin are inappropriate for routine care due to risk of allergy and anaphylaxis. Pharmacists can let patients know that the best way to treat minor cuts or scrapes is to clean them with mild soap and water and apply plain petrolatum if they need an emollient.24-26
DEALING WITH ENVIRONMENTAL EFFECTS
Many patients are highly motivated to protect the environment. Once consumed or applied, antibiotic metabolites and residue have to go someplace.27 That means they find their way down various drains and into our water supply. Most municipal sewage treatment plants were built decades ago, and few have the capacity to clean water as well as they should. Indirect effects of antibiotics in the environment include consequent development of multiresistant bacteria, death of aquatic environments, and harmful effects on birds and bees. Researchers indicate they have not yet identified all of antibiotics’ indirect long-term effects on the ecosystem.27 Educating patients on these concerns could help motivate them to improve their own antimicrobial stewardship.
CONCLUSION
Affixing appropriate auxiliary labels to prescription bottles is one way to remind patients that antibiotics have potential AEs. Spending a few minutes with a patient to explain why excessive antibiotic use poses a problem to individuals and the planet is another way to raise awareness. Although antibiotic stewardship is typically a multidisciplinary process, pharmacists can start that process.
